Abstract
Abstract Title: Prevalence Trends , Outcomes and Predictors of Mortality in Pulmonary Embolism
Background
Pulmonary embolism (PE) is the third most common vascular disease in the US, frequently underdiagnosed and potentially fatal condition where embolic material blocks one or more pulmonary arteries impairing blood flow. In this study, we aim to describe the prevalence, outcomes, and predictors of mortality of mechanical (MT) and surgical thrombectomy (ST).
Methods
This is a retrospective study using the Agency for Healthcare Research and Quality’s HCUP NIS data for 2010-2018. We used the ninth and tenth revision of the International Classification of Diseases, clinical modification codes (ICD-9-CM and ICD-10-CM) to identify patients admitted with primary diagnosis of PE (ICD-10-CM codes I26.02, I26.09, I26.92, I26.93, I26.94, I26.99, ICD-9-CM codes 415.11, 415.13, 415.19). We extracted demographics, hospital-level, and patient-level characteristics, defined the severity of comorbid conditions using Deyo modification of the Elixhauser-Comorbidity-Index. Primary outcomes were utilization trends of PE treated with MT and ST); secondary outcomes were mortality, discharge to facility, peri-procedural complications, and length of hospital (LOS) stay; tertiary outcome was to identify the predictors of in-hospital mortality.
Results
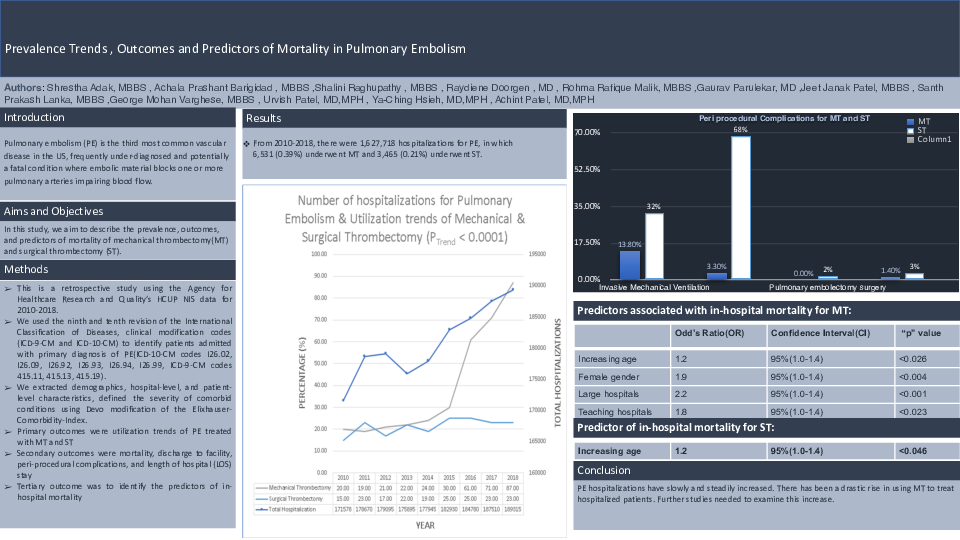
From 2010-2018, there were 1,627,718 hospitalizations for PE, which 6,531 (0.39%) underwent MT and 3,465 (0.21%) underwent ST. Utilization trend of MT increased from 336 (0.20%) in 2010 to 1,655 (0.87%) in 2018; the utilization trend of ST was 260 (0.15%) in 2010 and 430 (0.23%) in
2018. The unadjusted in-hospital mortality for MT was 9.1% and a mean LOS being 7(+/-0.3) days; for ST
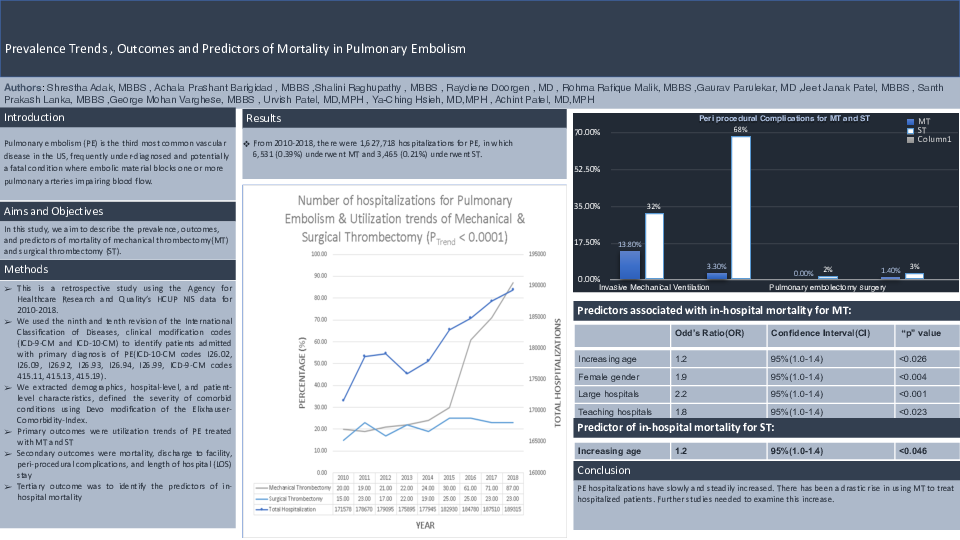
13.9% and a mean LOS 13(+/-0.4) days. Periprocedural complications for MT and ST: Invasive Mechanical Ventilation 13.8% and 32%, Cardiopulmonary Bypass 3.3% and 68.3%, pulmonary embolectomy surgery 1.7%; bleeding complications 1.4% and 3.4%Predictors associated with in-hospital mortality for MT: increasing age (OR 1.2, 95% CI 1.0-1.3, p<0.026), female gender (OR 1.9, 95% CI 1.2-2.8, p<0.004), large hospitals (OR 2.2, 95% 1.4-3.5, p<0.001), and teaching hospitals (OR 1.8, 95% CI 1.1-3.1, p<0.023). Predictor of in-hospital mortality for ST was increasing age (OR 1.2, 95% CI 1.0-1.4, p<0.046)
Conclusion
PE hospitalizations have slowly and steadily increased. There has been a drastic rise in using MT to treat hospitalized patients. Further studies needed to examine this increase.