Abstract
Alexander Louie1, Suresh Senan1, Pretesh Patel2, Bart Ferket3, Frank Lagerwaard1, George Rodrigues4, Joseph Salama2, Christopher Kelsey2, David Palma4, Myriam Hunink5
1VU University Medical Center, Amsterdam, Netherlands
2Duke University Medical Center, Durham, NC
3Harvard School of Public Health, Boston, MA
4London Regional Cancer Program, London, ON
5Harvard School of Public Health, Boston, MA
Purpose: The practice of treating a solitary pulmonary nodule (SPN) suspicious for Stage I NSCLC with stereotactic ablative radiotherapy (SABR) in the absence of pathologic confirmation of malignancy is becoming more common. In the absence of randomized evidence, the appropriate lung cancer prevalence threshold of when such a strategy is warranted can be informed using a decision modeling approach.
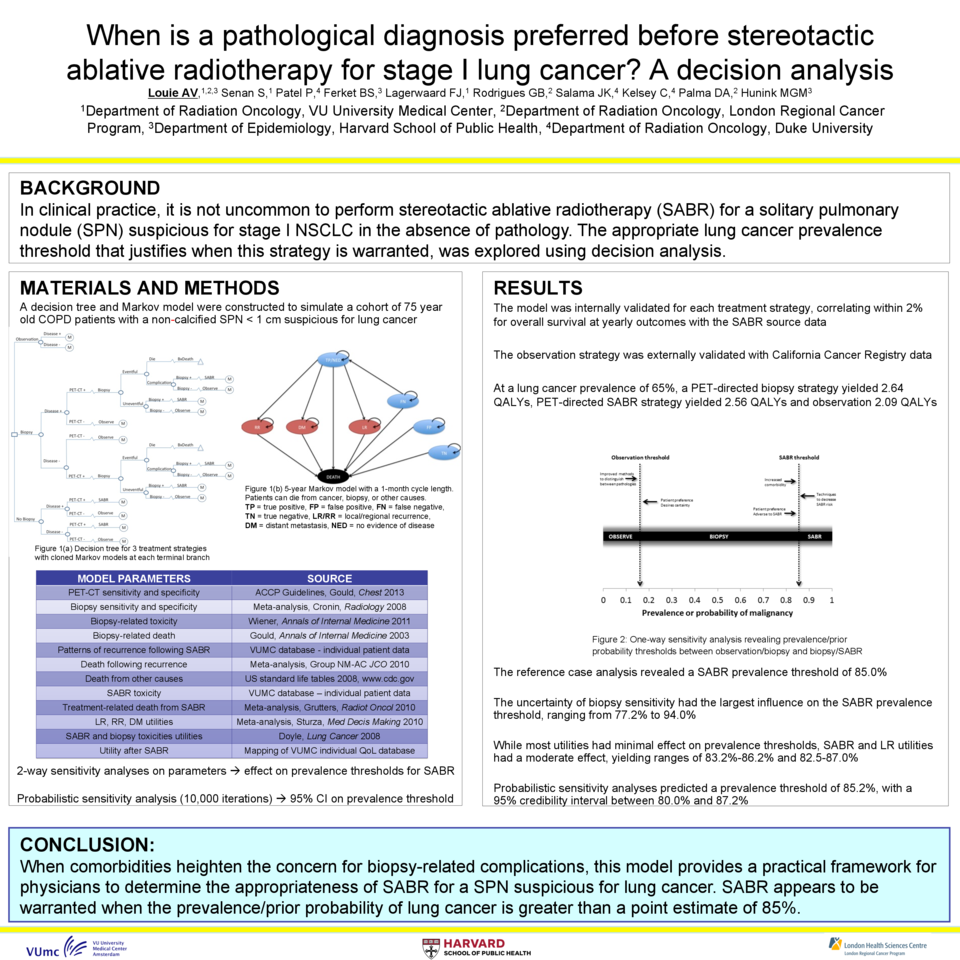
Materials and Methods: A decision tree and Markov model were constructed to evaluate the relative merits of observation, performing SABR without pathology, or performing a biopsy prior to SABR, when faced with a non-calcified SPN > 1cm in a 75-year-old patient at different lung cancer prevalences. Diagnostic characteristics, lung cancer utilities, as well as disease, treatment, and toxicity parameters were extracted from meta-analyses, guideline-based recommendations, and decision analyses. Toxicity and recurrence rates after SABR were obtained from a prospectively collected database of 382 patients receiving SABR for confirmed or suspected Stage I NSCLC. As utilities of early stage lung cancer patients treated with SABR have not been well studied, we employed mapping techniques to generate these from another 382 prospective individually-collected EORTC QLQ-C30 quality of life scores in the database. Deterministic sensitivity analyses on all model inputs were performed to inform the appropriate lung cancer prevalence threshold between treatment strategies. The effects of uncertainty in model parameters were evaluated through probabilistic sensitivity analysis (PSA), a technique in which parameter values are picked at random from a distribution for multiple iterations via Monte Carlo simulations. The model was validated internally with source data and externally with data from the California Cancer Registry. A five-year time horizon using a cycle length of one month was employed and quality adjusted life years (QALYs) were discounted at a rate of 3%.
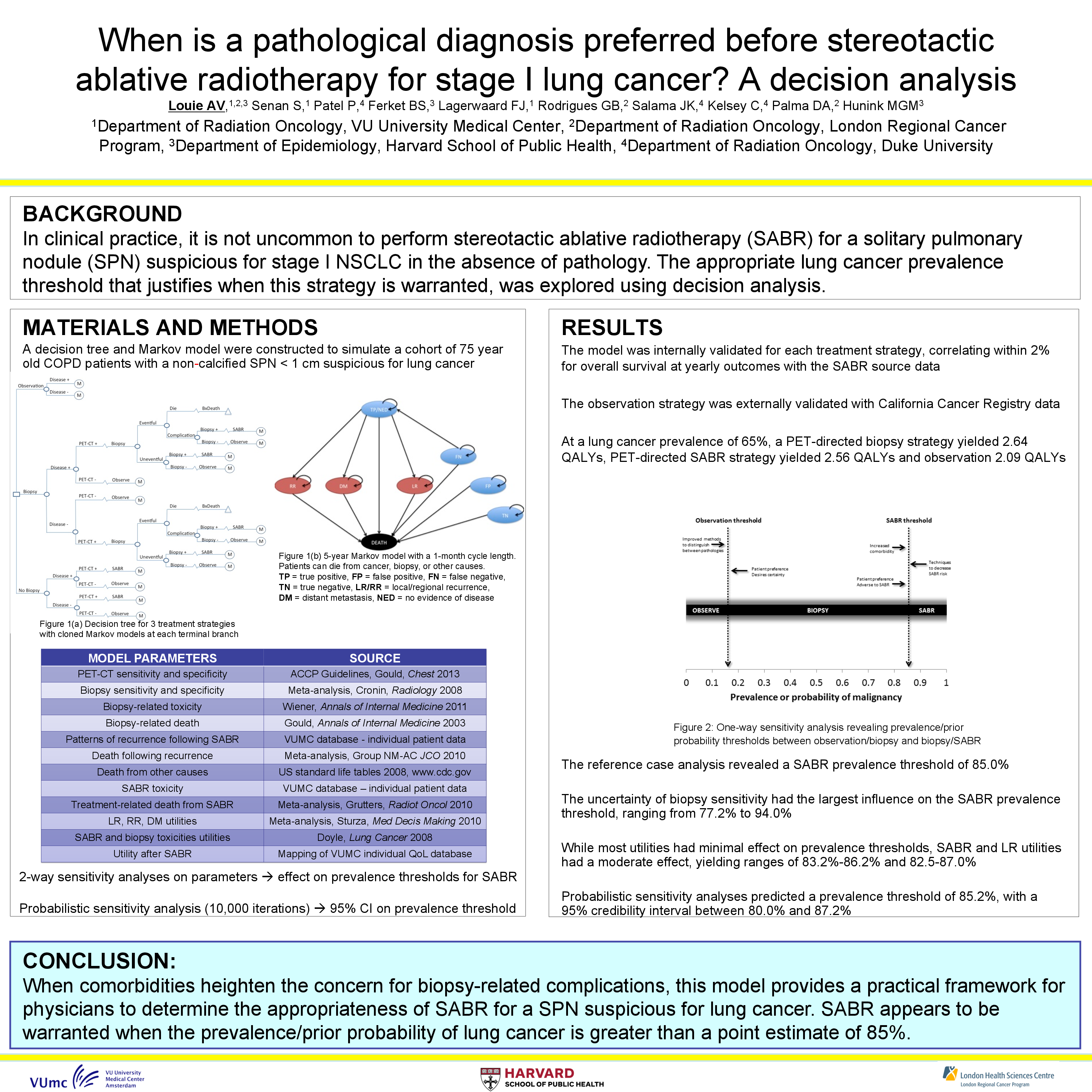
Results: At a lung cancer prevalence of 65%, performing a biopsy was the preferred treatment strategy, yielding 2.640 QALYs, compared to 2.563 and 2.086 for the no biopsy and observation strategies, respectively. The prevalence threshold between observation and performing a biopsy was 17.0%; and between performing SABR without pathology and performing a biopsy prior to SABR was 85.0%. The latter finding was confirmed on PSA (85.2%; 95% CI: 80.0%–87.2%). This predicted lung cancer prevalence threshold was most sensitive to the diagnostic sensitivity of transthoracic biopsy (range: 77.2–94.0%).
Conclusions: This model suggests that if there are concerns about increased morbidity related to biopsy for a SPN in an elderly and frail population, SABR is warranted as a treatment strategy when the prevalence of lung cancer exceeds a point estimate of 85%.