Abstract
H Bahig, D Simard, L Létourneau-Guillon, D Roberge, D Donath, P Wong, É Filion, D Béliveau-Nadeau, R Doucet, P Nicholson, L Masucci
CHUM, Montreal, QC
Purpose: Magnetic resonance (MR) imaging is essential in the assessment of tumour response following spine stereotactic body radiotherapy (SBRT). Morphologic changes post-spine SBRT remain poorly understood. The aim of this study was to assess early volumetric and signal intensity changes after spine SBRT and to correlate these changes to local control (LC).
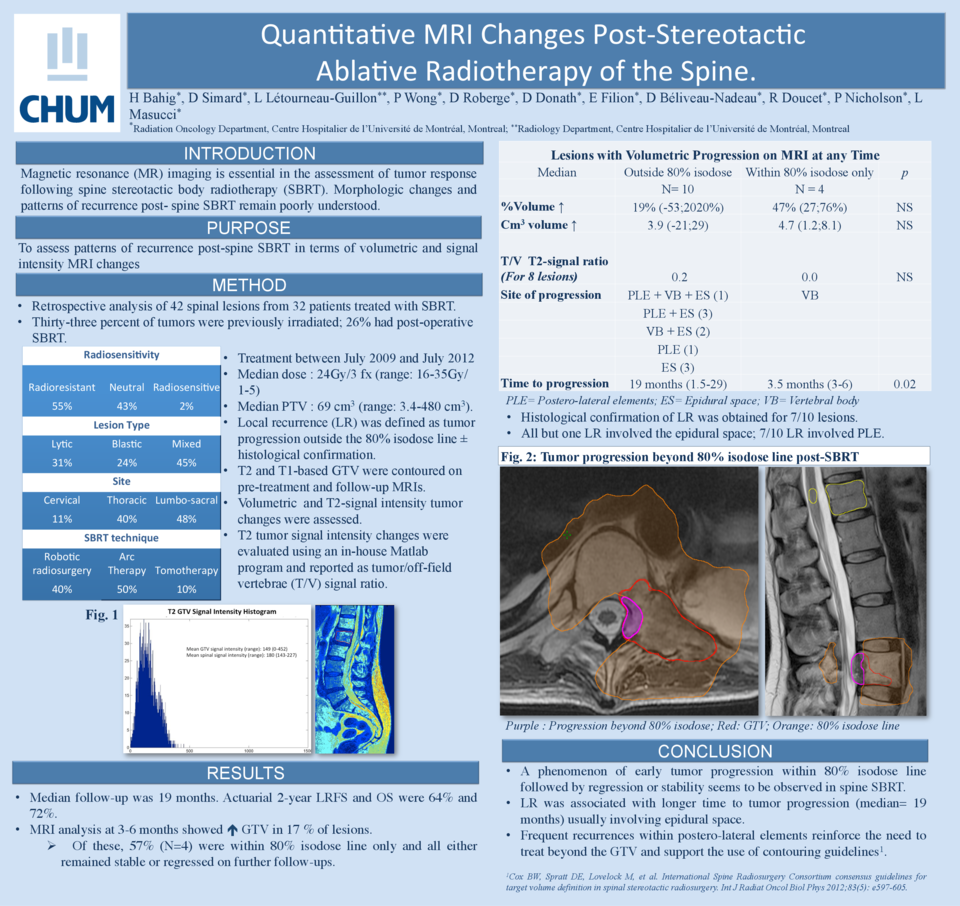
Materiel and Methods: T1 and T2-weighted non-contrast MR images of 30 spinal lesions from 27 patients treated with SBRT were retrospectively analyzed. Lesions were categorized as radioresistant (53%), neutral (43%) or radiosensitive (3%). Thirty-three percent of tumours were previously irradiated; 26% had post-operative SBRT. Lesions were either lytic (33%), blastic (23%) or mixed (44%). SBRT was delivered using robotic radiosurgery (53%), volumetric IMRT (37%) or helical tomotherapy (10%). Median dose was 24Gy in 3 fractions (range: 16-35Gy in 1-5) and median planning target volume was 58 cm3 (range: 3.4-480 cm3). T1 and T2-based gross tumour volumes (GTV) were contoured by a single observer on pre-treatment MRI and on follow-up MRIs. An in-house MatLab program was developed to analyze T2 signal changes using the spinal cord as reference signal intensity. Volume and T2-signal alterations at first follow-up (3-6 months) were correlated with LC. Patients with local recurrence (LR) had GTV growth followed by surgery with documented disease in surgical specimen.
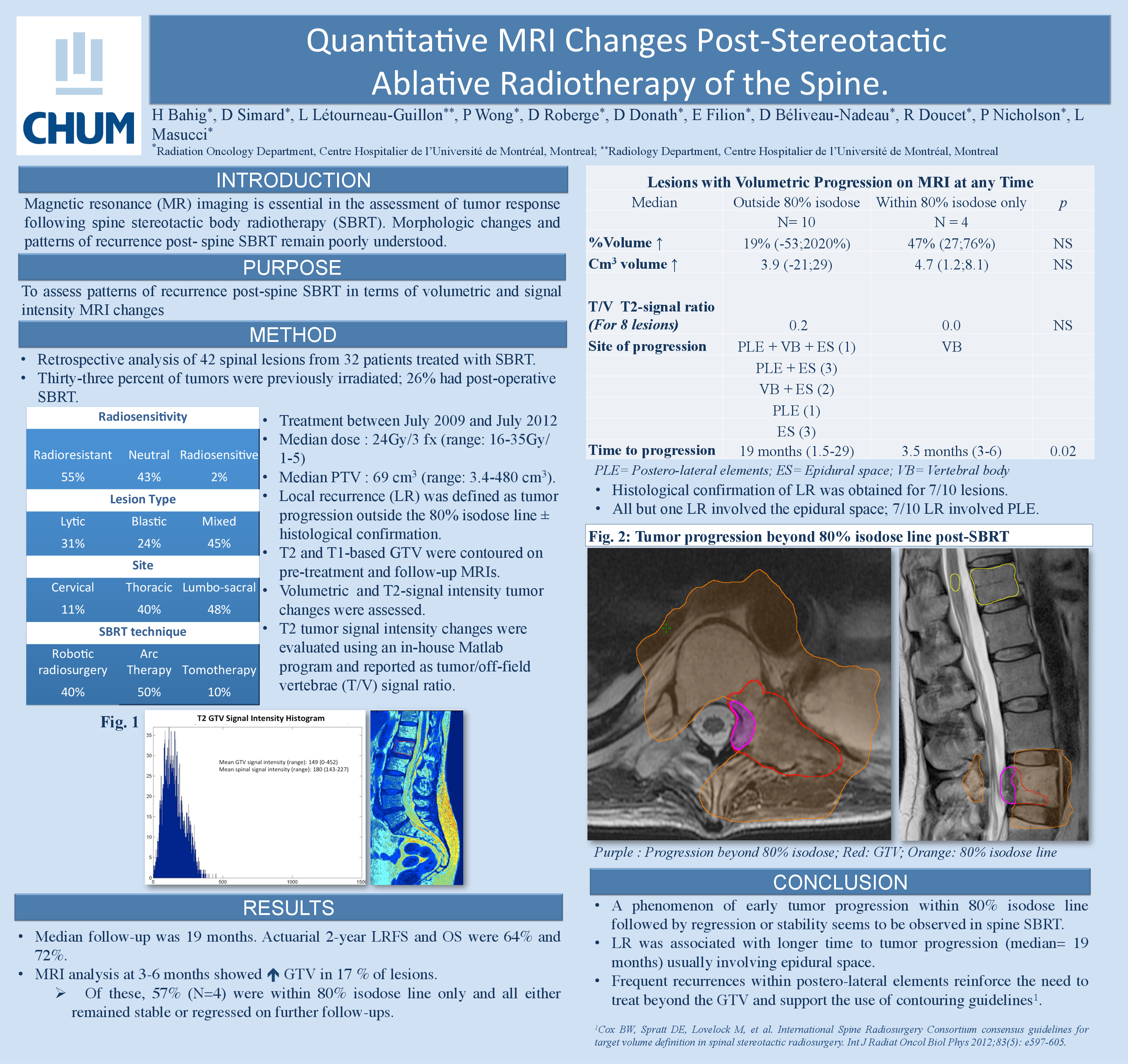
Results: Median follow-up was 15.2 months. Actuarial LC, disease-specific survival and overall survival were respectively 78%, 76% and 85% at one year and 46%, 45% and 79% at two years. Median time to LR was 17 months (range=1.5-24). Analysis on first MRI showed an increase in T1 and T2 GTV in 47% of lesions. Of these, 47% ultimately developed LR. All patients with LR presented increased GTV at 3-6 months. Of these, all but one had an increased GTV (median 28%, range=1; 290%) associated with reduced T/S signal ratio (median decrease -0.16, range=-0.04; -0.7); the remaining patient presented with 32% GTV increase and 0.6 T/S ratio increase. In patients with no LR at last follow up, 21% presented a GTV increase (median 4%, range=1; 57%) associated in all cases with an increased T/S ratio (median 0.7, range: 0.5; 1.34). Volume increase was generally more important in patients that ultimately did recur after surgical pathology confirmation (median 19% versus 4%, range=2; 205% versus 1; 57%). Decreased GTV was observed in 79% of lesions with no LR (median-13%, range= -2; -55%) associated with an increased T/S ratio in 63% of cases (median 0.5, range=0.3; 0.8) and decreased T/S ratio in 37% of cases (median-1.3, range=-0.1; -2.7).
Conclusions: Early (3-6 month) changes in T1 and T2 volume seem to correlate with subsequent local failure. Patients with what may be small increases in tumour volume on the first post-SBRT MRI should be followed more closely for LR. Early T2 signal changes do not appear to correlate with LC.