Abstract
Amandeep Taggar, Harold Lau, Gerald Lim, Robert Nordal, Rao Khan, Karen Breitman, Alana Hudson, David Spencer, Jon-Paul Voroney
Tom Baker Cancer Centre, Calgary, AB
Purpose: Stereotactic radiosurgery (SRS) is an important tool in management of brain metastases. Frameless SRS uses image guidance to deliver high dose radiation to the target volume, while being minimally invasive. Frameless techniques have improved patient comfort and allow flexibility in scheduling radiosurgery delivery. Previous case series have low patient numbers or short follow-up. In this study we report clinical outcomes and our centre's experience with SRS in treating newly diagnosed brain metastases.
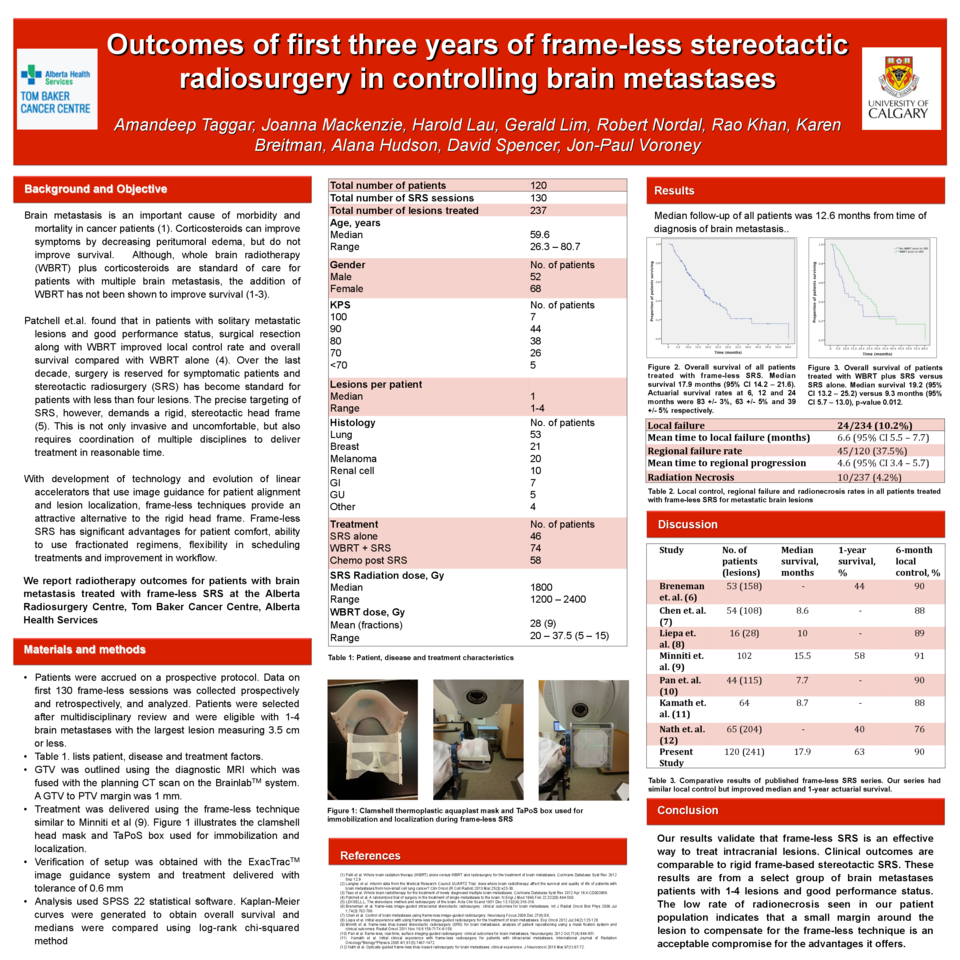
Materials and Methods: We reviewed electronic charts of all patients undergoing SRS at the Tom Baker Cancer Centre, Calgary, Alberta between June 2010 and September 2013. A total of 235 lesions in 120 patients were treated in 130 SRS sessions. Median age of patients undergoing SRS was 58.5 years (range 26-81). Median Karnofsky Performance Status (KPS) was 80 (range 60-100). Patients had non-small cell lung cancer (51), breast cancer (21), melanoma (20), renal cell carcinoma (10), colorectal cancer (seven) and others (13). Number of lesions treated in a single session ranged from one to four.
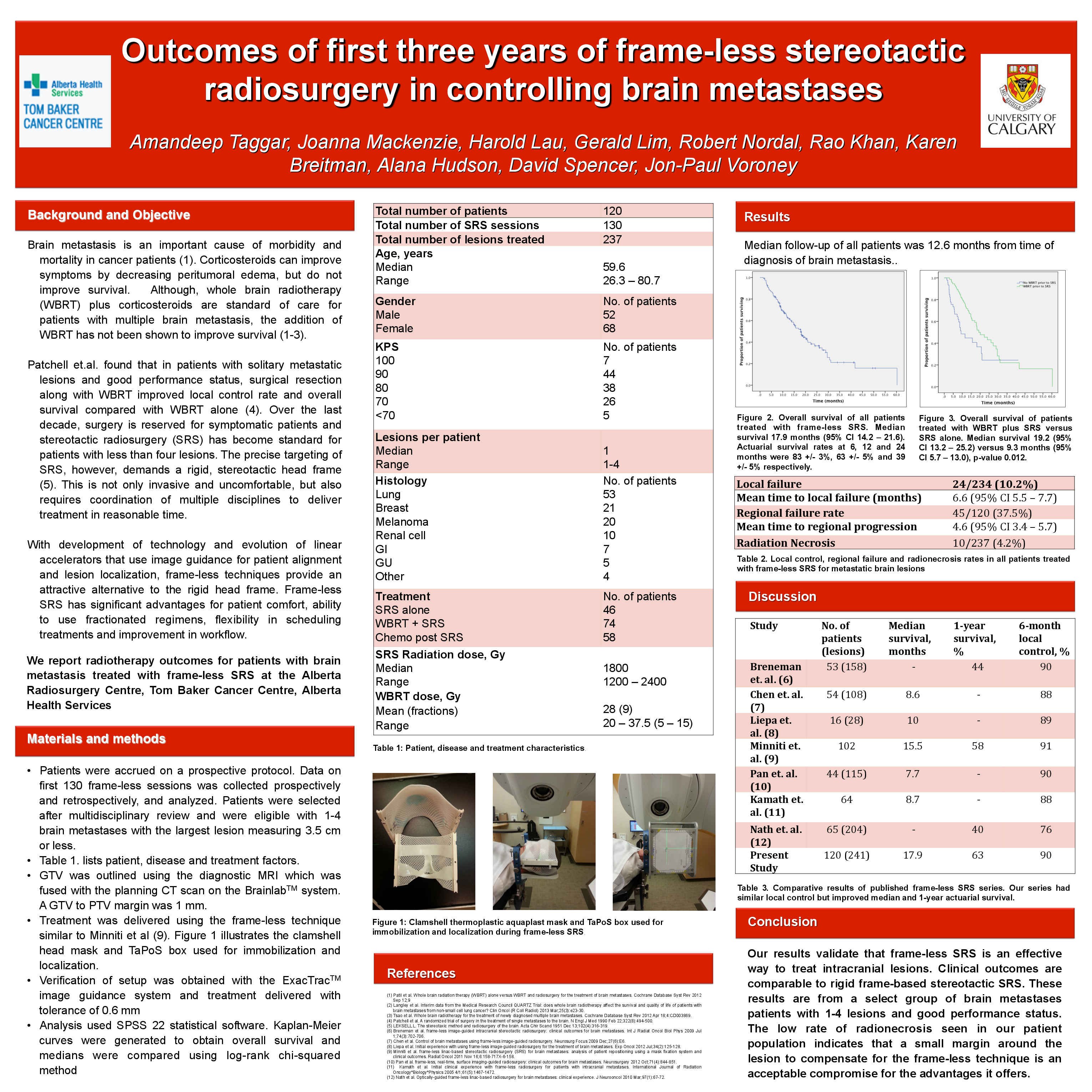
Results: Median follow up was 12.7 months (range 0-60). Overall median survival from the time of brain mets diagnosis was 18.2 months (95%CI 14-22 months) and 10.4 months from time of SRS (95% CI 7-13 months). Seventy-four (62%) patients received whole brain radiotherapy (WBRT) prior to SRS. Median survival from the time of brain mets diagnosis was 22.3 months for patients treated with WBRT plus SRS versus 9.3 months for patients treated with SRS (95% CI 14-30 months and 1-17 months respectively). Overall, fifty percent of patients received palliative chemotherapy after SRS (55% if KPS ≥80; 33% if KPS ≤70; no difference if prior WBRT). Median survival for patient who received chemotherapy was 22.3 months versus 12.3 months who did not. We identified local failure rate (within SRS site) of 11%, whereas 38% of patients had distant intracranial relapse; there was no difference between those who did or did not receive WBRT prior to SRS. Radionecrosis was identified in 8% of treated lesions.
Conclusions: This is so far the largest frameless SRS series. Our results are comparable if not better than previously reported. Frameless SRS is an effective, non-invasive option for patients with less than four metastatic lesions as well as patients with residual or growing lesions post WBRT. Patients who underwent chemotherapy post-SRS had better overall survival regardless of WBRT prior to SRS or number of lesions treated with SRS.