Abstract
Matthew Mason, Meredith Giuliani, Melanie Rose, Jennifer Deering, Shao Hui Huang, Haiyan Jiang, Brian O'Sullivan, Andrew Bayley, Jolie Ringash, John Cho, John Kim, John Waldron, Andrew Hope University of Toronto, Toronto, ON
Purpose: To determine if patient reported outcomes (PROs) correlate with short and intermediate-term clinical support requirements during chemoradiotherapy (CRT) for head and neck (H&N) cancer patients.
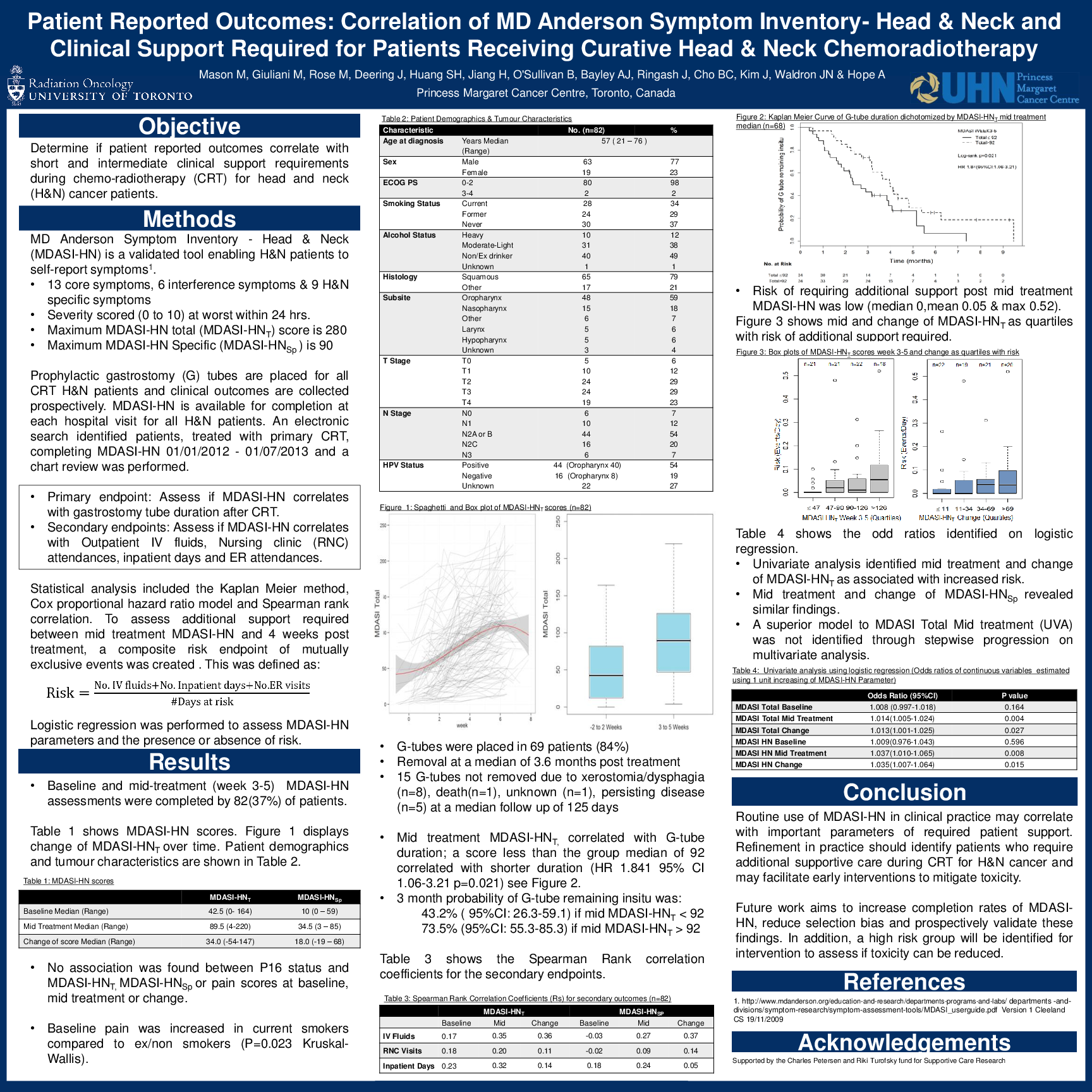
Materials and Methods: Based on available evidence for our environment, our tertiary referral cancer center routinely sites prophylactic gastrostomy (G) tubes in H&N patients receiving CRT. All patients are asked to electronically complete MDASI-HN©,a validated PRO assessment, in English pre-, during, and post-treatment. Twenty-eight items (scored at worst within 24 hours on a scale from 0 to 10) of which nine are H&N specific are documented. The maximum total score is 280 for MDASI-HN (MDASI-HNT) and 90 for H&N specific elements (MDASI-HNSp). The study period was from January 2012 to July 2013. Medical record review was completed for patients receiving CRT who completed MDASI-HN at both baseline (within two weeks of treatment start) and mid-treatment (weeks 3-5). Data collected during treatment included: G-tube duration, nursing clinic attendances, outpatient IV fluid provision and inpatient stay duration. G-tube dependency was calculated using the Kaplan Meier method and the effect of MDASI-HN scores on duration assessed by Cox regression. Spearman correlation coefficients (Rs) were calculated for the other variables
Results: Of 221 patients treated with primary CRT, 134 (61%) completed two or more MDASI assessments during treatment. This analysis included 82 patients having both baseline and mid-treatment MDASI-HN scores. Median age was 57 (range: [21, 76]). Median MDASI-HNT at baseline was 42.5 [0, 164] and 89.5 [4, 220] at mid-treatment. The median MDASI-HNT change was 34.0 [-54, 147]. Median MDASI-HNSp was 10 [0,59] and 34.5 [3, 85] for baseline and mid treatment respectively with a median change of 18.0 [-19, 68]. Intravenous fluid requirements correlated with change in both MDASI-HNT (Rs=0.358) and MDASI-HNSp (Rs=0.372). Inpatient admission days correlated with baseline MDASI-HNT (Rs=0.227). Of the 82 patients, 69 (84%) had G-tube placement with removal at a median of 3.6 months post treatment. For this subgroup of patients only mid treatment MDASI-HNT, using Cox regression, correlated with G-tube duration; a score less than the group median of 92 correlated with shorter duration (HR 1.841 95% CI 1.055-3.213 p=0.032).
Conclusions: Routine use of MDASI-HN in clinical practice correlates with important parameters of patient support, for example intravenous fluid requirements, during CRT. Its refinement in practice should identify patients who require additional supportive care during CRT for H&N cancer and may facilitate early interventions to mitigate toxicity.