Abstract
Background: Black women/birthing people are 3 times more likely to experience a pregnancy-related death than their non-Hispanic White counterparts. In 2022, the Black maternal mortality rate was 49.5 per 100,000 live births compared to 19.0 per 100,000 live births among White women. Furthermore, Black women/birthing people experienced severe maternal complications 27% more than their counterparts. Such disparities may be due to racism, discrimination, and disproportionate rates of chronic disease. Given that 80% of maternal deaths are preventable, this warrants the need to identify areas for improvement within clinical settings.
Objectives: The aims of this community-partnered study were to 1.) assess the sense of security, support, and safety, as well as perceived experiences and treatment of Black women/birthing people who received perinatal care from UCLA, and 2.) center the voices of Black women/birthing people and communities to identify opportunities for quality improvement and health education within the UCLA Health system.
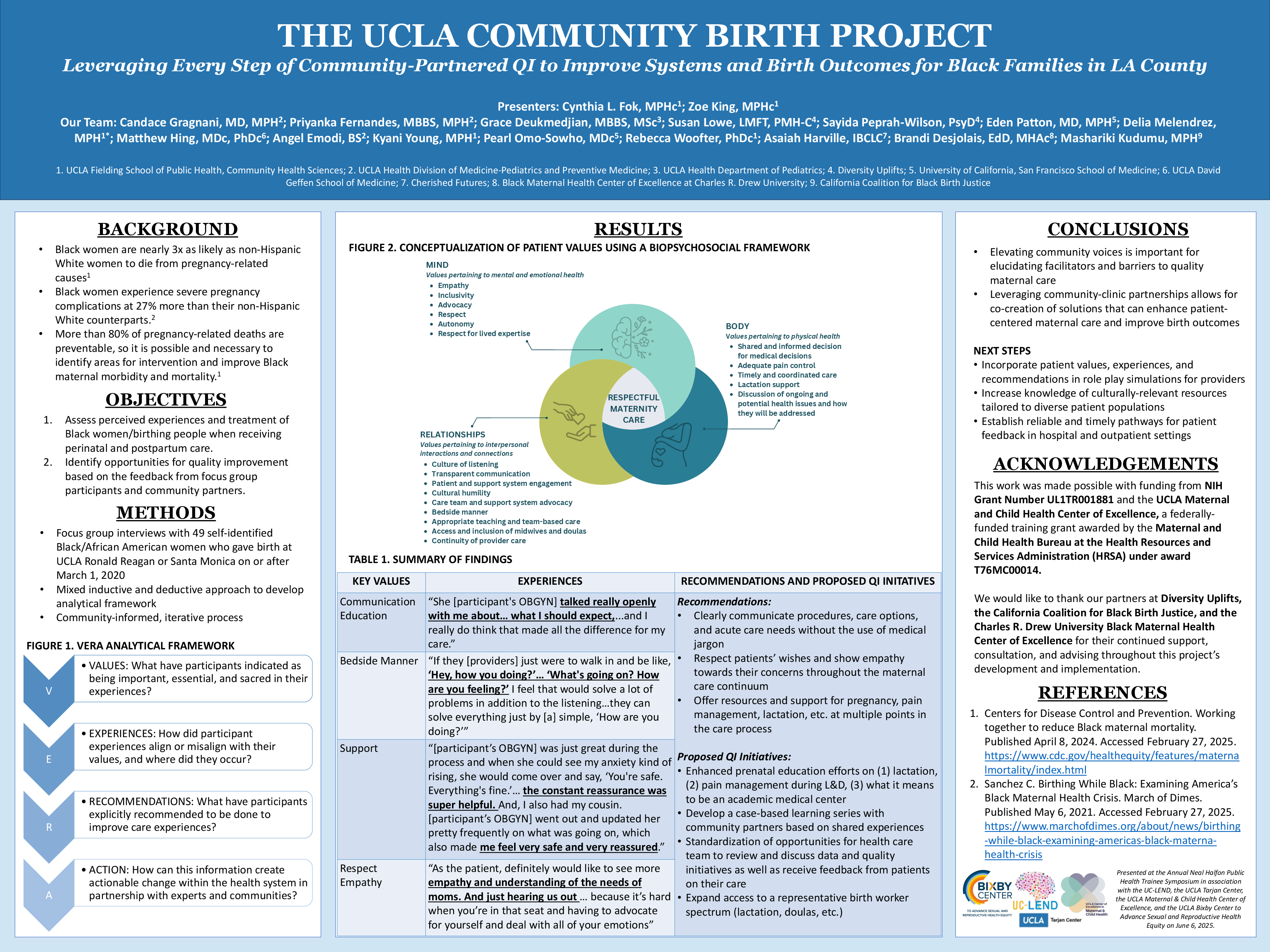
Methods: Ten focus groups were conducted among 49 self-identified Black and/or African American women/birthing people who gave birth at UCLA Ronald Reagan or Santa Monica on or after March 1, 2020. Focus group interviews were held in-person (3) and virtually (7) and designed to elicit participants’ experiences across the maternal care continuum (i.e., prenatal, labor and delivery, postpartum, and lactation care). A semi-structured design allowed for exploration of themes related to patient values. An original analysis framework entitled VERA (Values, Experiences, Recommendations, and Actions) was used to deductively and inductively code focus group transcripts for recurrent themes. Iterative feedback from community partners was incorporated throughout the study.
Results: Our findings show that participants had diverse experiences with maternal care at UCLA Health. Common patient values included transparent communication, support, respect, bedside manner, and bias/discrimination. Negative experiences across the maternal care continuum were often attributed to poor patient-provider communication and bedside manner, a perceived lack of respect and empathy, and perceived provider biases. Positive experiences were often attributed to receiving adequate provider support, being listened to and respected, and having autonomy to make decisions. These patient values are conceptualized using a biopsychosocial framework, wherein respectful maternity care cannot be achieved without holistically addressing patient needs. Participant recommendations for improvements at UCLA Health reflected many of these values.
Conclusion: The insights from this study underscore the value of centering the voices of Black communities in understanding the gaps in care and improving patient experiences. Further, the VERA framework provided a new approach to translating patient experiences into actionable, patient-centered initiatives. As such, participant feedback will guide institutional quality improvement initiatives centered on delivering respectful maternity care at UCLA Health. This may include the development of provider training/resources that highlight patient-centered values, clinical workflows that streamline care across the maternal care continuum, and patient resources that include vital information on maternity care. These community-informed initiatives will drive progress in the delivery of respectful maternal care.