Abstract
Introduction
Diabetic foot infections are a serious complication of diabetes mellitus, often leading to ulcerations, gangrene, and osteomyelitis. Poor circulation, compromised immune response, and peripheral neuropathy, which reduces the sensation of pain and injury in the extremities, contribute to infection progression. Early recognition and treatment are critical in preventing limb amputation.
Objective
This clinical image case report aims to highlight the clinical presentation, diagnosis, and management of a diabetic foot infection complicated by osteomyelitis.
Methodology
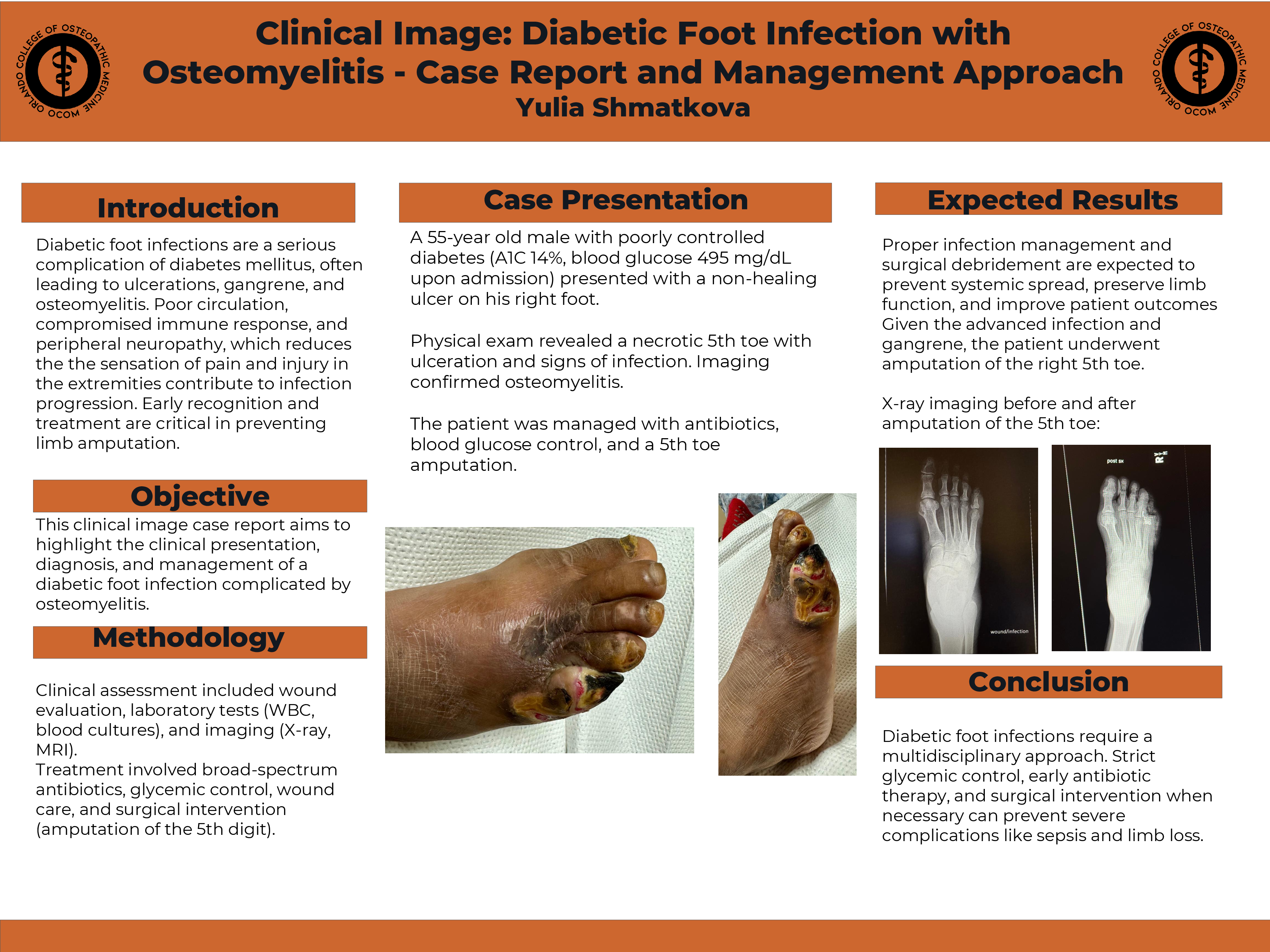
Clinical assessment included wound evaluation, laboratory tests (WBC, blood cultures), and imaging (X-ray, MRI). Treatment involved broad-spectrum antibiotics, glycemic control, wound care, and surgical intervention (amputation of the 5th digit).
Case Presentation
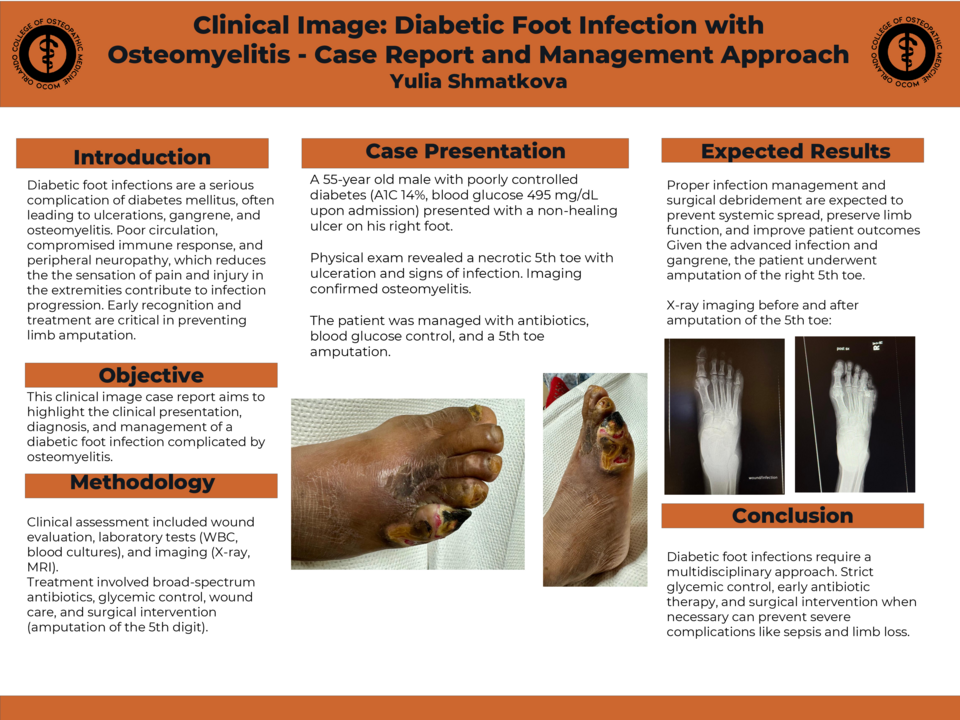
A 55-year old male with poorly controlled diabetes (A1C 14%, blood glucose 495 mg/dL upon admission) presented with a non-healing ulcer on his right foot. Physical exam revealed a necrotic 5th toe with ulceration and signs of infection. Imaging confirmed osteomyelitis. The patient was managed with antibiotics, blood glucose contorl, and a 5th toe amputation.
Expected Results
Proper infection management and surgical debridement are expected to prevent systemic spread, preserve limb function, and improve patient outcomes. Given the advanced infection and gangrene, the patient underwent amputation of the 5th toe.
Conclusion
Diabetic food infections require a multidisciplinary approach. Strict glycemic control, early antibiotic therapy, and surgical intervention when necessary can prevent severe complications like sepsis and limb loss.