Abstract
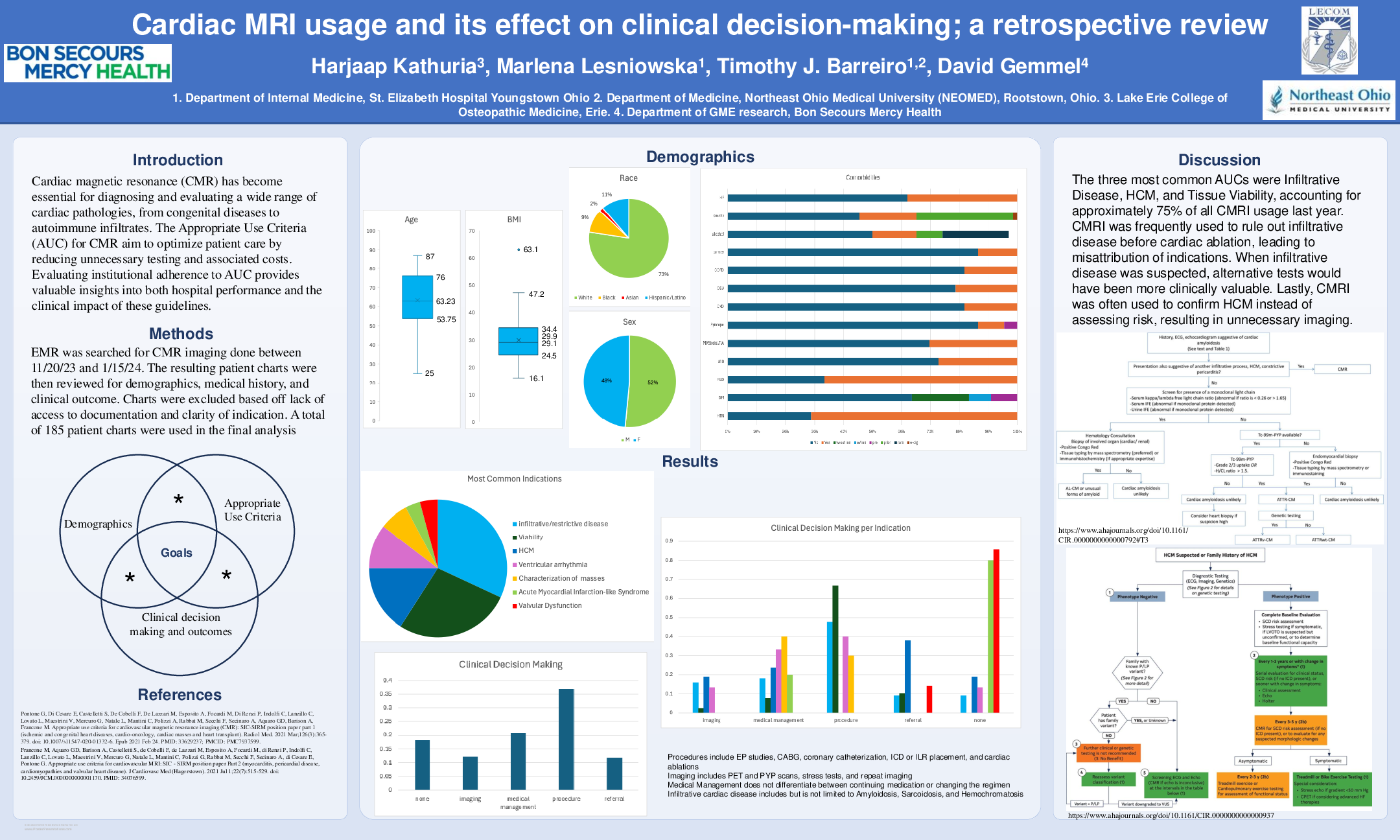
Cardiac magnetic resonance (CMR) has become essential for diagnosing and evaluating a wide range of cardiac pathologies, from congenital diseases to autoimmune infiltrates. The Appropriate Use Criteria (AUC) for CMR aim to optimize patient care by reducing unnecessary testing and associated costs. Evaluating institutional adherence to AUC provides valuable insights into both hospital performance and the clinical impact of these guidelines. A retrospective review of electronic medical records at St. Elizabeth Hospital Youngstown was conducted for patients who underwent CMR imaging between November 20, 2023, and November 15, 2024. The study assessed AUC adherence and the impact of CMR on clinical decision-making, defined as whether the diagnostic information led to a change in medical management, further imaging, or a referral to a specialist. A total of 222 patients were scanned during this period, with 87% of scans meeting class A or B AUC recommendations and 55% experiencing some change in medical management. The most common reason for requesting CMR was to rule out restrictive (infiltrative) cardiomyopathy (23%), with cardiac amyloidosis as the primary differential diagnosis. Tissue viability assessments and hypertrophic cardiomyopathy (HCM) were the second and third most common indications. Notably, none of the patients suspected of cardiac amyloidosis were diagnosed, resulting in no change in medical management. Overall, our findings highlight commendable adherence to AUC for CMR at our institution, with clinical decision-making influenced by approximately half of the imaging results. However, further diagnostic advancements may be needed to improve the identification of conditions such as cardiac amyloidosis.