Abstract
Background & Introduction
Healthcare providers enter the medical field with the mission to treat and heal patients, yet they increasingly face workplace violence that jeopardizes their physical and mental well-being. The World Health Organization (WHO) estimates that 38% of healthcare workers worldwide experience physical violence in their careers. A Press Ganey report states that two nurses are assaulted every hour in the U.S. Emergency department (ED) staff are particularly vulnerable, as 50% of emergency physicians report experiencing physical assault in the past year (WHO, 2022; Press Ganey, 2022). Violence includes verbal and physical assaults, threats, sexual harassment, stalking, and bullying, often arising from patient and family members. Beyond physical harm, workplace violence has devastating psychological effects.
Objective
This study examines the prevalence of workplace violence in the emergency department and its psychological impact on healthcare workers.
Methods
A convenience sample of emergency department staff—including physicians, nurses, non-physician providers, and techs—was surveyed. Researchers utilized a combination of self-developed questionnaire to assess exposure to workplace verbal, physical, and sexual violence and PCL-5 PTSD Checklist (Weathers et al., 2013). Data were collected through an anonymous, self-reported survey.
Results
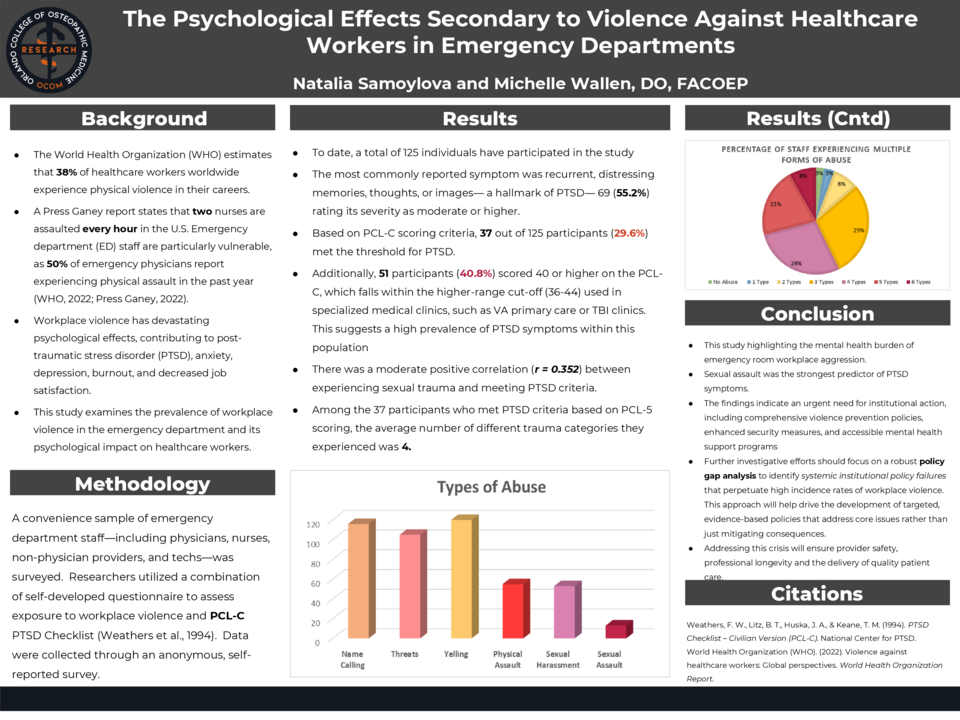
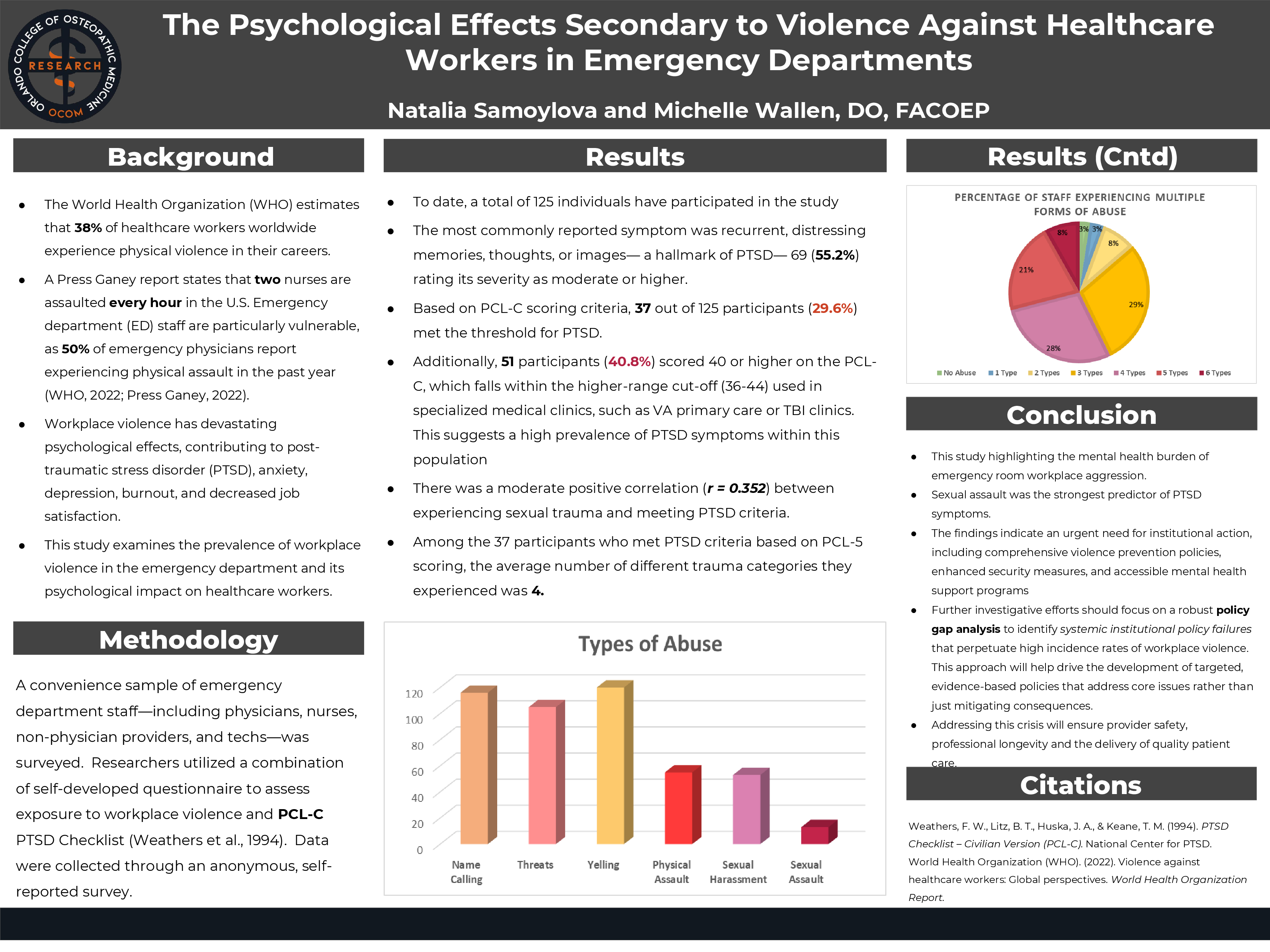
To date, a total of 125 individuals have participated in the study. Verbal aggression was the most frequently reported type of violence, followed by threats, physical assaults, and sexual harassment. The most commonly reported symptom was recurrent, distressing memories, thoughts, or images, with 69 participants (55.2%) rating its severity as moderate or higher. Based on PCL-5 scoring criteria, 37 out of 125 participants (29.6%) met the threshold for PTSD. This means that nearly one-third of respondents reported experiencing symptom severity consistent with a PTSD diagnosis, according to DSM-5 guidelines. Among those, there was a moderate positive correlation (r = 0.352) between experiencing sexual trauma and meeting PTSD criteria. Among the 37 participants who met PTSD criteria based on PCL-5 scoring, the average number of different trauma categories they experienced was 4.
Conclusion
Workplace violence in healthcare settings is highly prevalent and is associated with significant psychological distress, including PTSD symptoms. A notable percentage of participants met the DSM-5 PTSD symptom criteria, highlighting the mental health burden of workplace aggression. Sexual assault was the strongest predictor of PTSD symptoms, suggesting that targeted interventions are needed to mitigate trauma exposure and support affected employees. The findings indicate an urgent need for institutional interventions, including comprehensive violence prevention policies, enhanced security measures, de-escalation training, and accessible mental health support programs. Addressing this crisis is critical to ensuring both provider safety, professional longevity the delivery of high-quality patient care.