Abstract
Introduction:
Ectopic pregnancy (EP) is a serious pregnancy complication that occurs when a gestational sac implants outside the uterus, most commonly in the fallopian tubes. However, Cesarean scar ectopic pregnancies (CSEPs), a rare form of EP, occur in the previous Cesarean section scar and have an increasing incidence due to the rising rate of Cesarean deliveries. CSEPs are challenging to diagnose and pose significant risks, including rupture and hemorrhage, which can lead to maternal death. This case report highlights the diagnostic and treatment challenges posed by CSEPs.
Case Report:
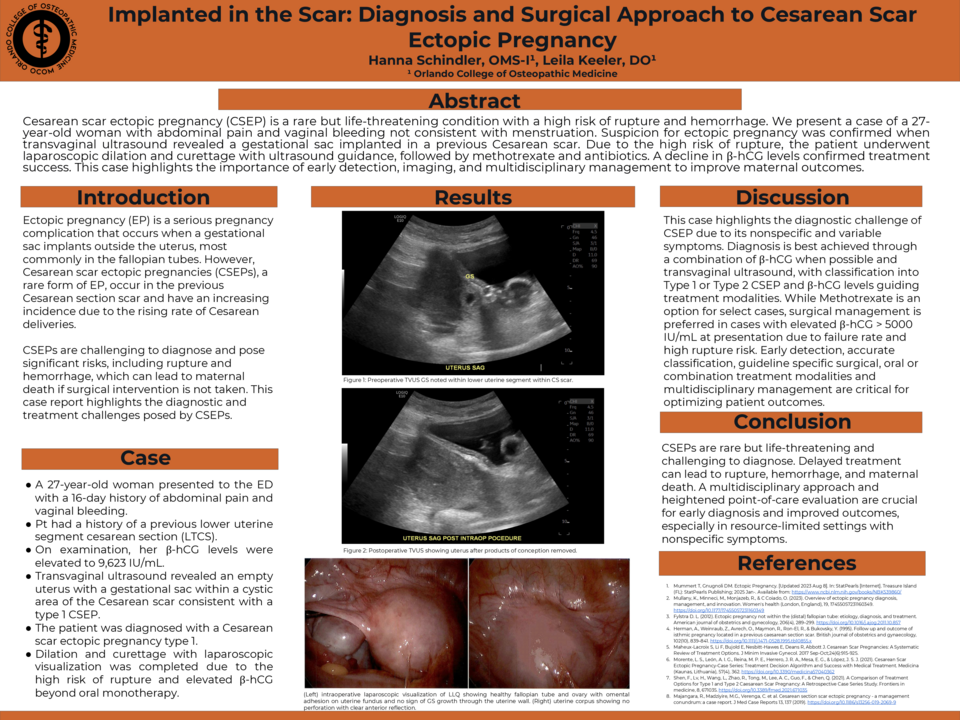
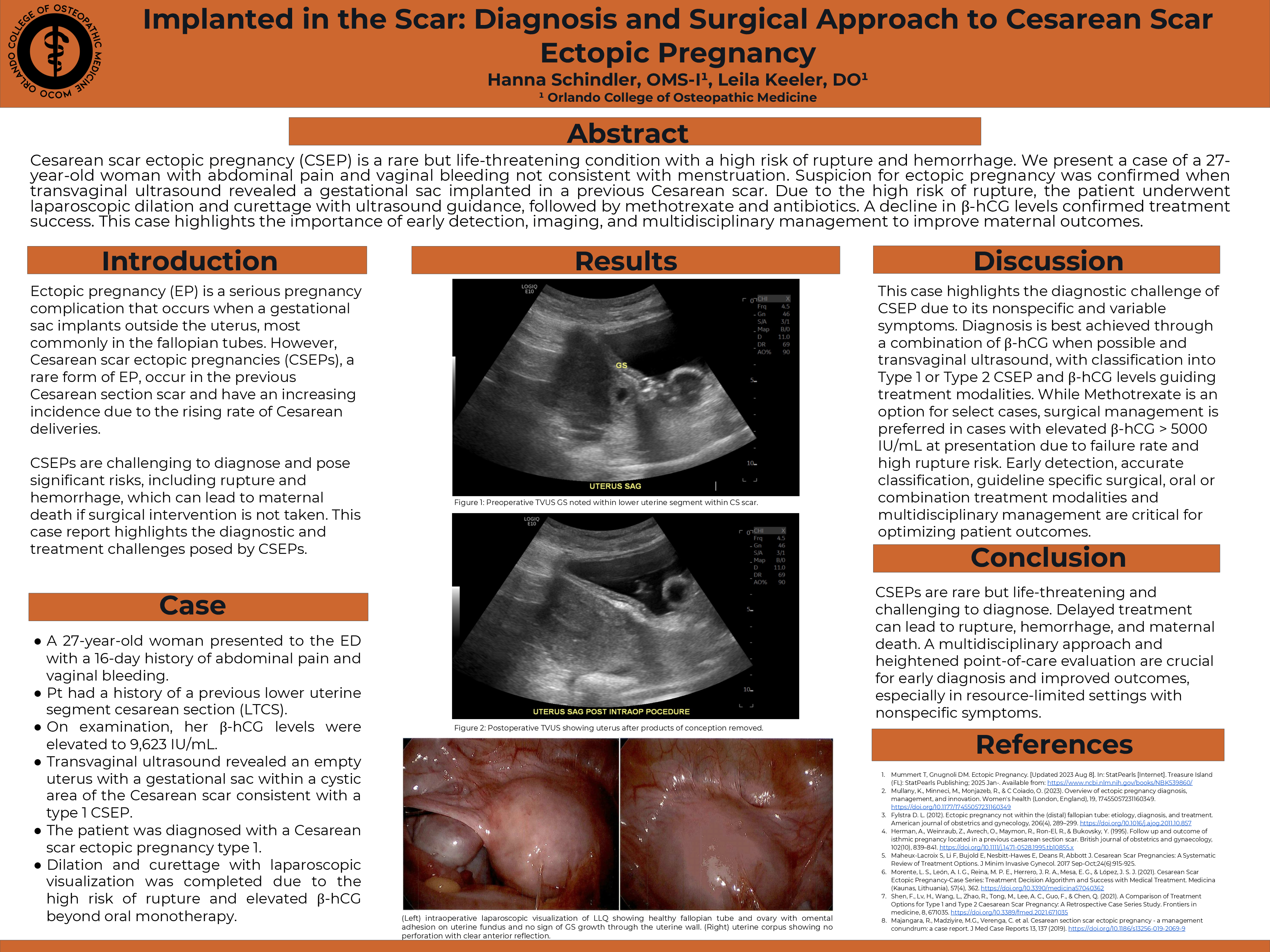
A 27-year-old woman presented to the emergency department (ED) with a 16-day history of abdominal pain and vaginal bleeding, initially believed to be her menstrual period. She had a history of one previous lower uterine segment cesarean section (LTCS). On examination, her β-hCG levels were elevated, and transvaginal ultrasound revealed an empty uterus with a gestational sac within a cystic area of the Cesarean scar. The patient was diagnosed with a Cesarean scar ectopic pregnancy. Surgical resection was recommended due to the high risk of rupture, and the patient underwent laparoscopic surgery with dilation and curettage for gestational sac removal. Postoperative management included methotrexate, antibiotics, and analgesia. A follow-up β-hCG test showed a significant decline, confirming resolution of the ectopic pregnancy. At her two-week follow-up, the patient remained asymptomatic with no further vaginal bleeding, and ultrasound imaging confirmed the absence of retained products of conception.
Discussion:
The analysis of this case report was conducted through a retrospective review of clinical presentation, laboratory findings, imaging studies, and surgical intervention. Key diagnostic indicators such as β-hCG trends, transvaginal ultrasound (TVUS) imaging, and intraoperative findings were critically examined to determine the classification and severity of the cesarean scar ectopic pregnancy (CSEP). The typing system for CSEP was applied to assess implantation site characteristics, guiding the decision-making process for intervention. The differential diagnosis process was analyzed to highlight the challenges in distinguishing CSEP from other first-trimester complications such as early pregnancy loss, uterine rupture, or retained products of conception. Furthermore, the risk-benefit evaluation of treatment modalities, including medical versus surgical management, was conducted to justify the chosen intervention. Postoperative outcomes and recurrence risks were also assessed to provide insight into the long-term implications of CSEP management. This case contributes to the growing body of literature on early recognition, classification, and surgical decision-making for cesarean scar pregnancies, emphasizing the importance of multidisciplinary collaboration and standardized diagnostic protocols to improve patient outcomes.
Conclusion:
CSEPs are a rare and life-threatening complication of pregnancy that require timely diagnosis and intervention. Early detection through transvaginal ultrasound and appropriate multidisciplinary management are critical to prevent adverse outcomes. Increased awareness of this condition and a structured approach to diagnosis and treatment can improve maternal health outcomes, especially in resource-limited settings.