Abstract
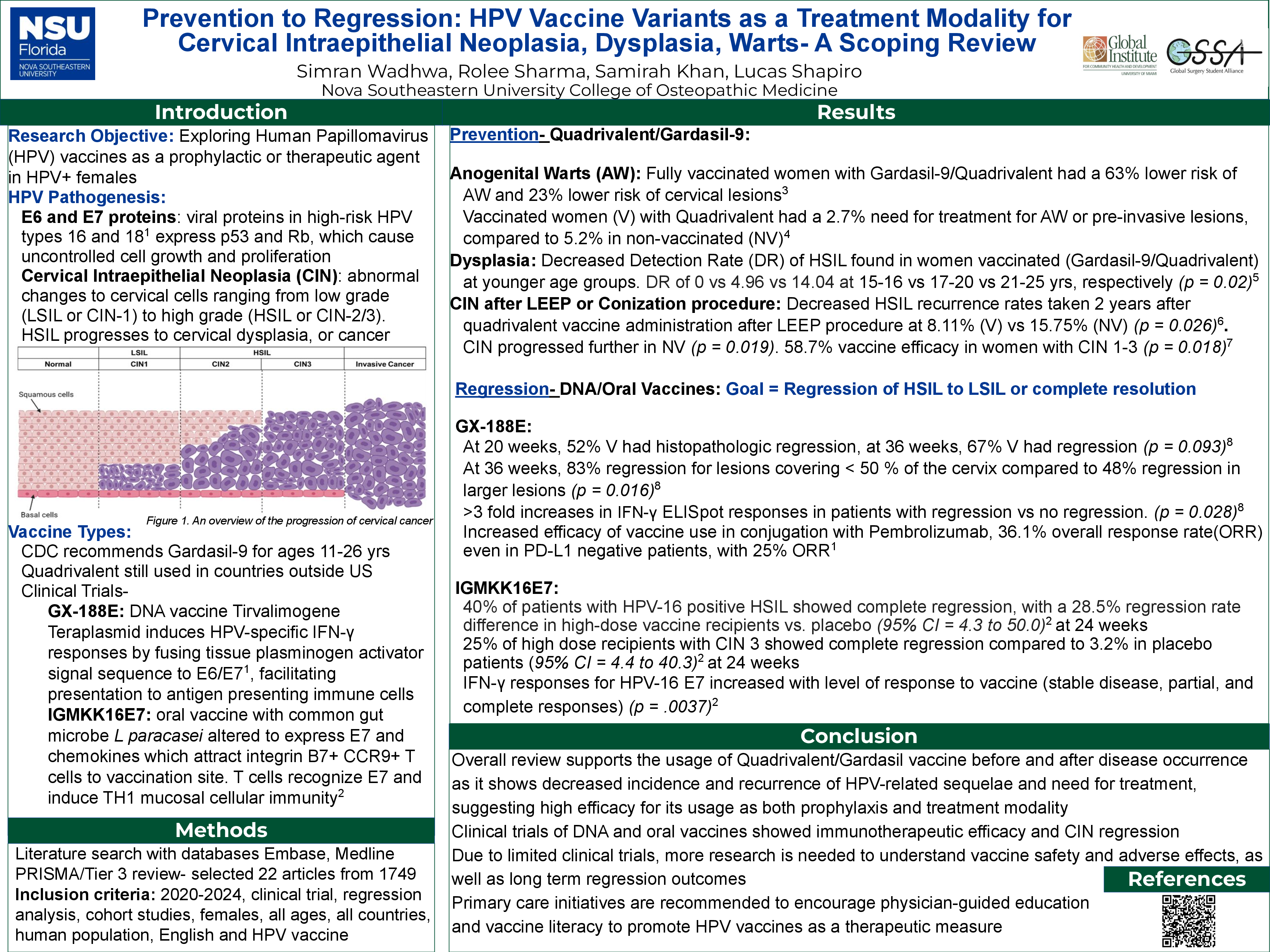
Human Papillomavirus (HPV) infection poses a significant public health concern globally as the leading cause of cervical cancer. The HPV vaccine is widely known for preventing high-risk strains of HPV, and is now being studied for its therapeutic potential as a treatment modality after the diagnosis of HPV has been made. The objective of this scoping review is to review recent literature to understand the usage of the HPV vaccine as a prophylactic or therapeutic agent for females who have been diagnosed with HPV, and are suffering from cervical intraepithelial neoplasia (CIN), dysplasia or anogenital warts (AW). This review also emphasizes the importance of health literacy and positive impact of HPV education on treatment outcomes.
A literature search was performed using the databases Embase and Medline. PRISMA guidelines were followed with the following inclusion criteria: journal articles published from 2020-2024, clinical trial, regression analysis or cohort studies, females of all ages, all countries, and HPV vaccine utilization. Initial literature searches yielded 1749 articles which were narrowed down to 22 articles selected after a rigorous Tier 3 review. This review process is demonstrated in a PRISMA diagram. This review found that in management of cervical/vulvar cancer and precancerous lesions, HPV vaccination was shown to decrease incidence with a minimum of one dose given, even after dysplasia has occurred. This correlation has the strongest effect in women in the 20s-30s age group. Vaccinated women under the age of 21 were also seen to be 54% less likely to be hospitalized for HPV associated issues. Retrospective studies demonstrated that there was a decreased incidence of AW in patients vaccinated against HPV. The quadrivalent vaccine was 74% effective as a prophylactic treatment for preventing disease while the bivalent was not considered effective. Along with the vaccine, organized vaccination programs are seen to be effective at decreasing rates of dysplasia which lead to AW and precancerous lesions.
In women with cervical biopsies displaying CIN, quadrivalent or Gardasil-9 vaccines were administered as a treatment after CIN diagnosis. Subsequent biopsies showed significant regression compared to non-vaccinated women, as well as lower rates of persisting/recurring high-grade squamous intraepithelial lesion (HSIL) in women who underwent cervical conization and/or Loop Electrosurgical Excision Procedure (LEEP) procedure. Clinical trials of new therapeutic vaccines to be given as a treatment were also reviewed. Phase II of a clinical trial of IGMKK16E7 (lacticaseibacillus paracasei) oral vaccine expressing cell surface-HPV 16 E7 antigen demonstrated a statistically significant improved rate difference of 28.5% in high-dose recipients vs. placebo for HPV-16 positive HGSIL. GX-188E is a DNA vaccine that has been increasingly studied as well. Clinical trial evidence shows that it is more effective for lesions covering less than 50% of the cervix, and effective to use in conjugation with a monoclonal antibody that binds to PD-1 called Pembrolizumab, even in PD-1 negative patients. Additional research is needed to further understand the efficacy of new therapeutic vaccines. Studies must also determine if decreased cervical dysplasia rates are due to the HPV vaccine alone or earlier timing of HPV testing and/or increased public health efforts for vaccination and HPV propaganda.