Abstract
Introduction: Hemophagocytic lymphohistiocytosis (HLH) occurring subsequent to Hodgkin lymphoma (HL) is a seldom encountered complication, with an estimated incidence of 8.9%. This case is a notable illustration of HL evolving into T-cell/histiocyte-rich large B-cell lymphoma before manifesting as secondary HLH. The rarity and variety of clinical presentations highlight the difficulty in making an accurate diagnosis and putting into practice effective treatment plans. The lack of literature on the best management strategies further exacerbates this problem, as approximately 66.8% of HLH patients pass away within a median period of 5.1 months.
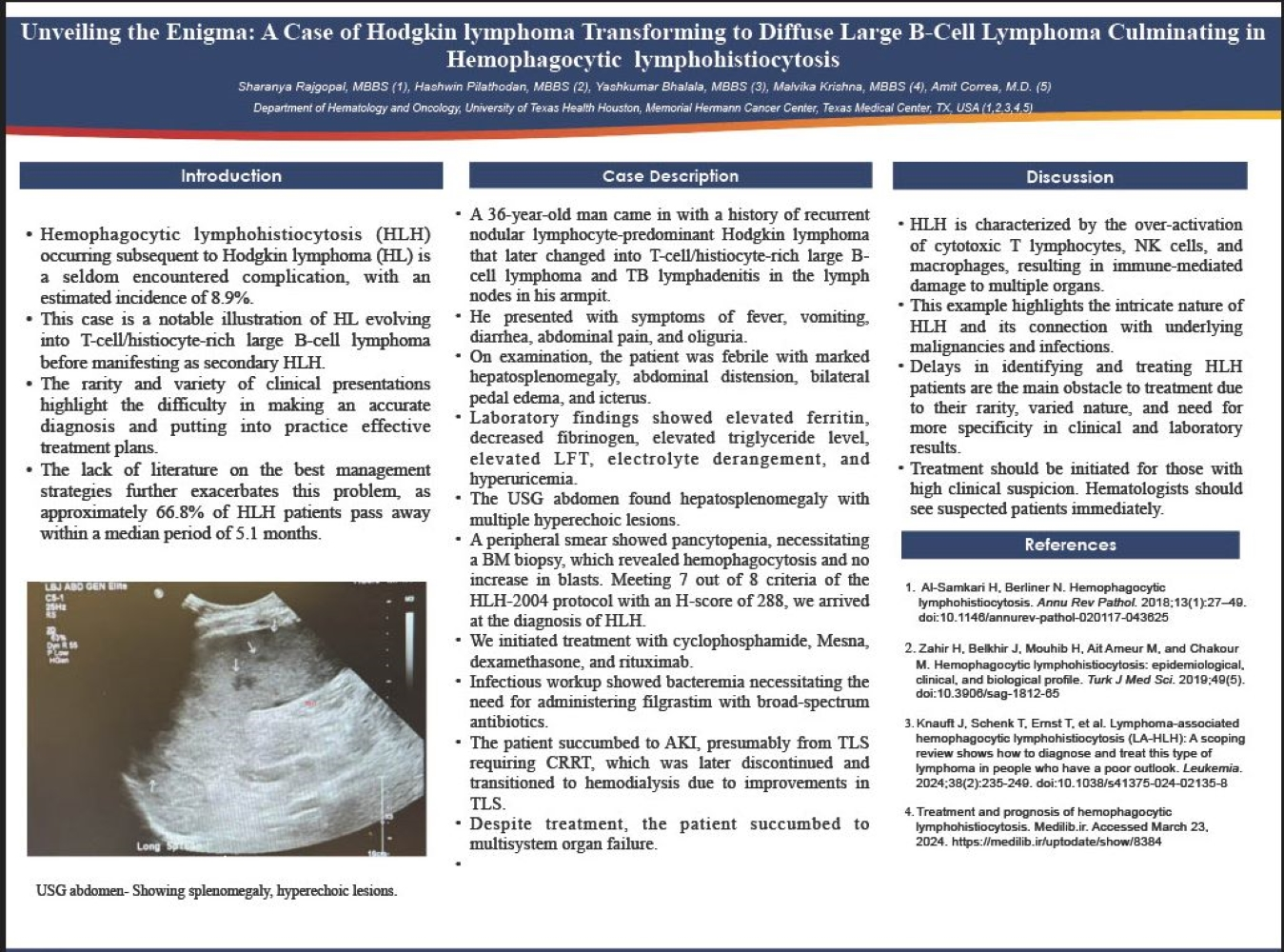
Case report: A 36-year-old man came in with a history of recurrent nodular lymphocyte-predominant Hodgkin lymphoma that later changed into T-cell/histiocyte-rich large B-cell lymphoma and TB lymphadenitis in the lymph nodes in his armpit. He presented with symptoms of fever, vomiting, diarrhea, abdominal pain, and oliguria. On examination, the patient was febrile with marked hepatosplenomegaly, abdominal distension, bilateral pedal edema, and icterus. Laboratory findings showed elevated ferritin, decreased fibrinogen, elevated triglyceride level, elevated LFT, electrolyte derangement, and hyperuricemia. The USG abdomen found hepatosplenomegaly with multiple hyperechoic lesions. A peripheral smear showed pancytopenia, necessitating a BM biopsy, which revealed hemophagocytosis and no increase in blasts. Meeting 7 out of 8 criteria of the HLH-2004 protocol with an H-score of 288, we arrived at the diagnosis of HLH. We initiated treatment with cyclophosphamide, Mesna, dexamethasone, and rituximab. Infectious workup showed bacteremia necessitating the need for administering filgrastim with broad-spectrum antibiotics. The patient succumbed to AKI, presumably from TLS requiring CRRT, which was later discontinued and transitioned to hemodialysis due to improvements in TLS. Despite treatment, the patient succumbed to multisystem organ failure.
Discussion: HLH is characterized by the overactivation of cytotoxic T lymphocytes, NK cells, and macrophages, resulting in immune-mediated damage to multiple organs. This example highlights the intricate nature of HLH and its connection with underlying malignancies and infections. Delays in identifying and treating HLH patients are the main obstacle to treatment due to their rarity, varied nature, and need for more specificity in clinical and laboratory results. Treatment should be initiated for those with high clinical suspicion. Hematologists should see suspected patients immediately.