Abstract
Pneumocystis pneumonia (PCP) is a leading cause of AIDS-associated morbidity and mortality, particularly in individuals who are not diagnosed with HIV until they are profoundly immunosuppressed. The diagnosis can be challenging and may require invasive procedures like bronchoscopy. Microscopic exam of bronchoalveolar lavage (BAL) is diagnostic of PCP, but the use of non-invasive methods like serum 1,3-beta-D-glucan (BDG) assay has been proposed more recently. Here, we discuss a case of PCP in a newly diagnosed HIV patient with a negative BDG assay.
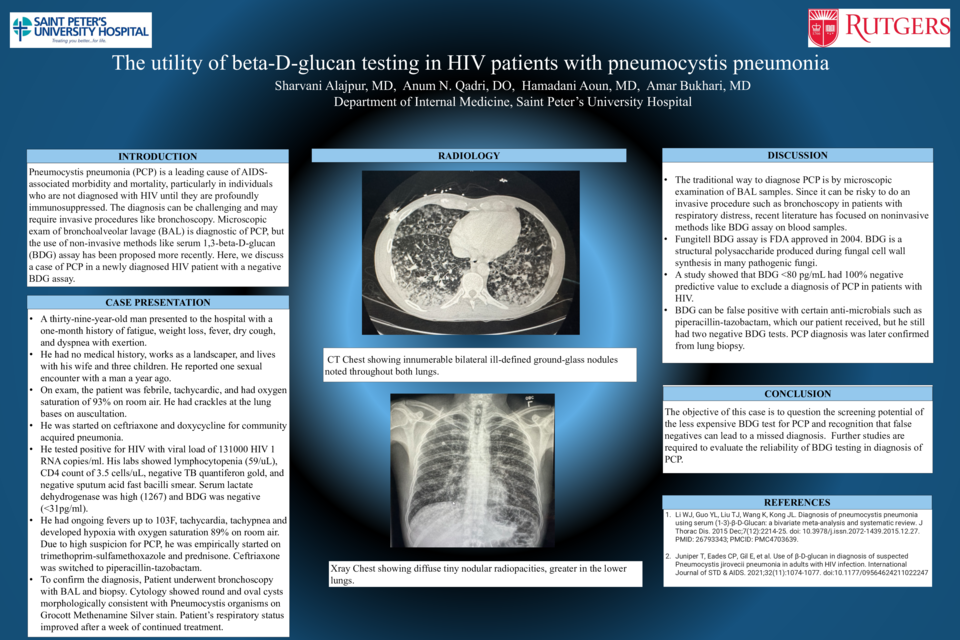
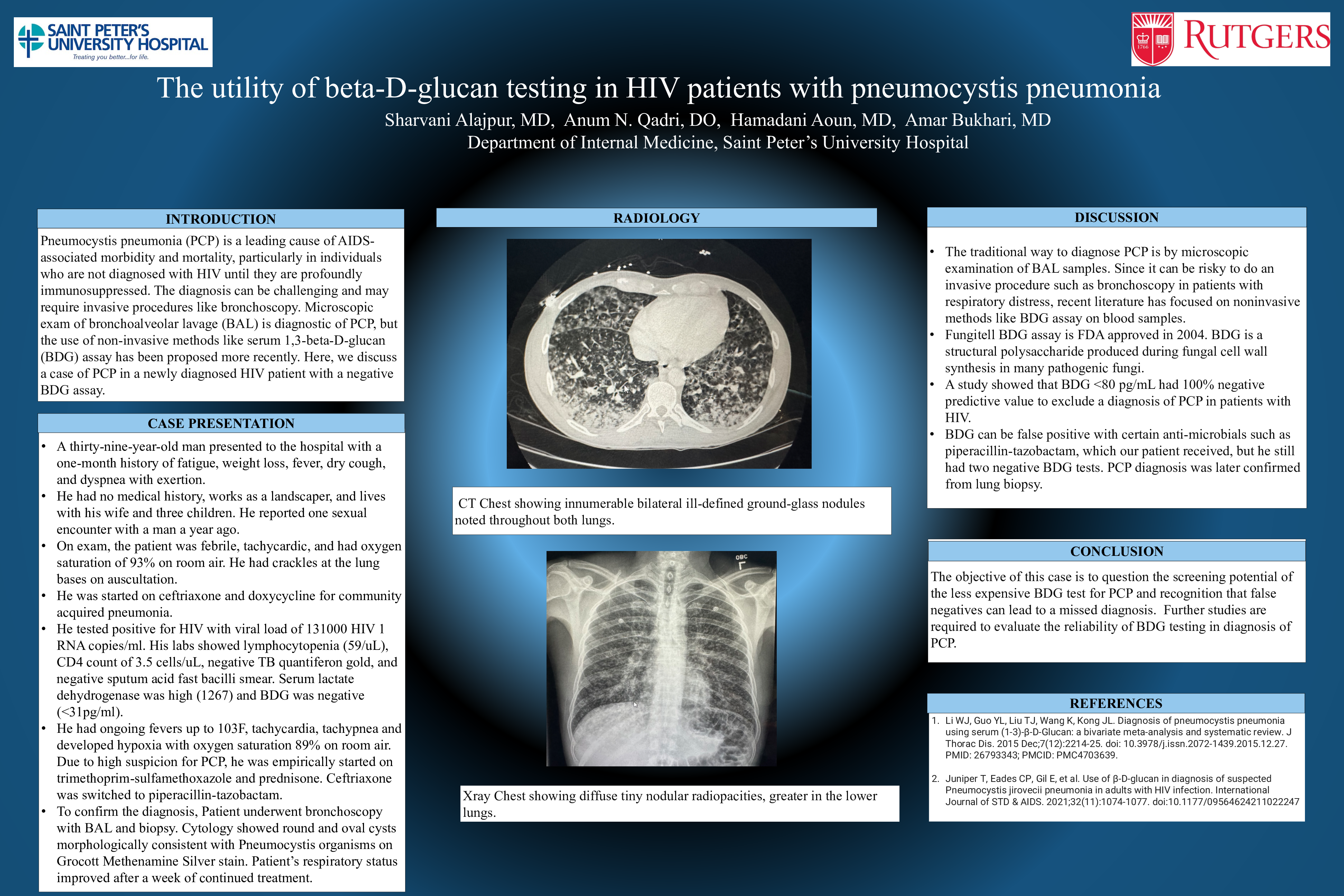
A thirty-nine-year-old man presented to the hospital with a one-month history of fatigue, weight loss, fever, dry cough, and dyspnea with exertion. He had no medical history, works as a landscaper, and lives with his wife and three children. He reported one sexual encounter with a man a year ago. On exam, the patient was febrile, tachycardic, and had oxygen saturation of 93% on room air. He had crackles at the lung bases on auscultation, extensive white plaques on his tongue, upper palate and posterior oropharynx, and no skin rashes. Chest x-ray showed diffuse bilateral nodular radiopacities, greater in the lower lungs. CT chest revealed diffuse bilateral ground glass opacities concerning for fungal or mycobacterial infection. He was started on ceftriaxone and doxycycline for community acquired pneumonia and fluconazole for esophageal candidiasis. He tested positive for HIV with viral load of 131000 HIV 1 RNA copies/ml. His labs showed lymphocytopenia (59/uL), CD4 count of 3.5 cells/uL, negative TB quantiferon gold, and negative sputum acid fast bacilli smear. Serum lactate dehydrogenase was high (1267) and BDG was negative (<31pg/ml). He had ongoing fevers up to 103F, tachycardia, tachypnea and developed hypoxia with oxygen saturation 89% on room air. Due to high suspicion for PCP, he was empirically started on trimethoprim-sulfamethoxazole and prednisone. Ceftriaxone was switched to piperacillin-tazobactam. To confirm the diagnosis, Patient underwent bronchoscopy with BAL and biopsy. Cytology from the BAL and lung biopsy showed round and oval cysts morphologically consistent with Pneumocystis organisms on Grocott Methenamine Silver stain. Patient’s respiratory status improved after a week of continued treatment.
The traditional way to diagnose PCP is by microscopic examination of BAL samples. Since it can be risky to do an invasive procedure such as bronchoscopy in patients with respiratory distress, recent literature has focused on noninvasive methods like BDG assay on blood samples. A study showed that BDG <80 pg/mL had 100% negative predictive value to exclude a diagnosis of PCP in patients with HIV. BDG can be false positive with certain anti-microbials such as piperacillin-tazobactam, which our patient received, but he still had two negative BDG tests. PCP diagnosis was later confirmed from lung biopsy. The objective of this case is to question the screening potential of the less expensive BDG test for PCP and recognition that false negatives can lead to a missed diagnosis.