Abstract
Introduction: Hashimoto's encephalopathy, also known as steroid-responsive encephalopathy associated with autoimmune thyroiditis, is a rare condition. We present a case of a patient with a history of rheumatoid arthritis who presented with new-onset seizure and psychotic features, and was eventually diagnosed with autoimmune encephalitis associated with Hashimoto’s thyroiditis.
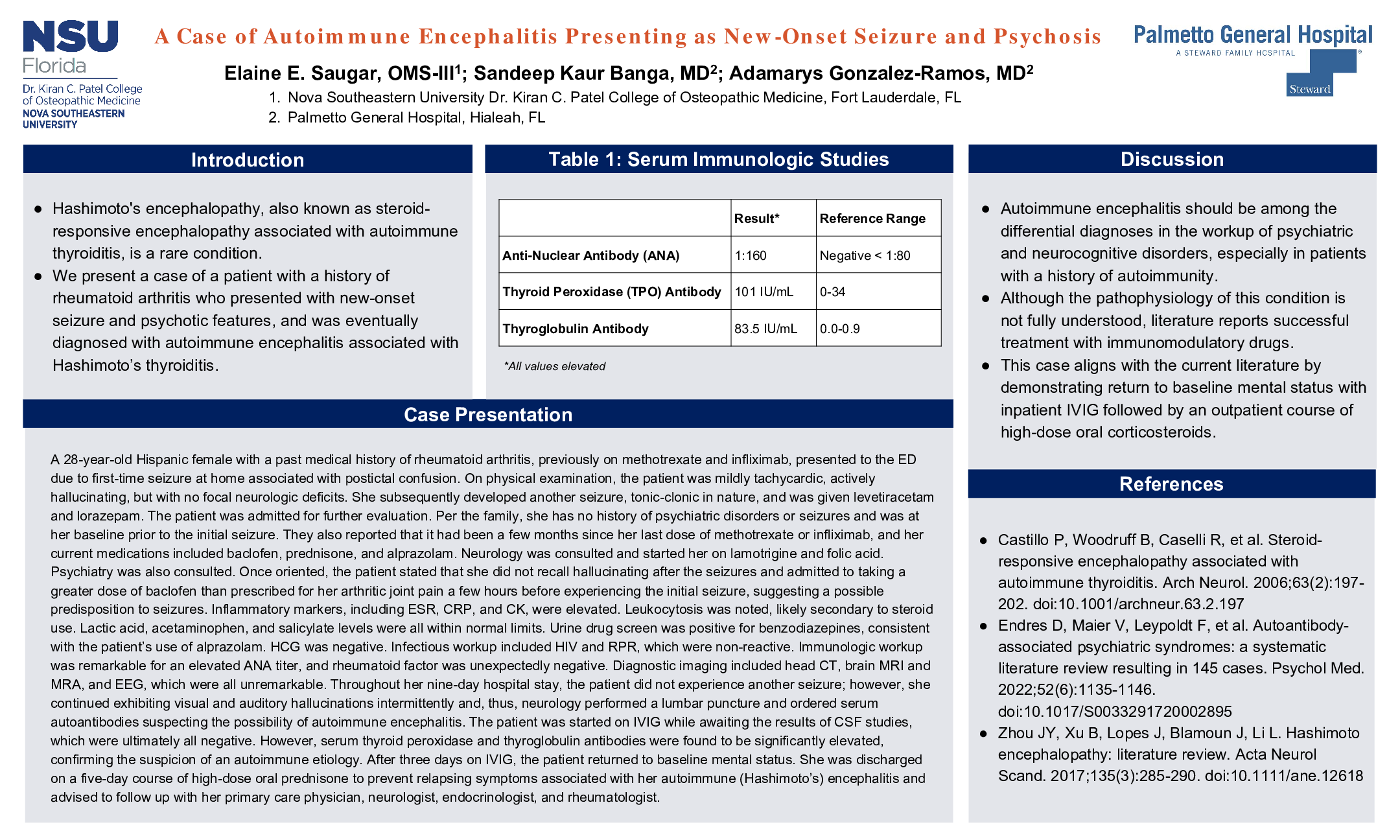
Case Description: A 28-year-old Hispanic female with a past medical history of rheumatoid arthritis presented to the ED due to first-time seizure and postictal confusion. On physical examination, the patient was mildly tachycardic, actively hallucinating, but with no focal neurologic deficits. She subsequently developed another seizure, tonic-clonic in nature, and was given levetiracetam and lorazepam. She was admitted for further evaluation. Per the family, she has no history of psychiatric disorders or seizures and was at her baseline prior to the initial seizure. They also reported that it had been a few months since her last dose of methotrexate or infliximab, and her current medications included baclofen, prednisone, and alprazolam. Neurology was consulted and started her on lamotrigine and folic acid. Psychiatry was also consulted. Once oriented, the patient stated that she did not recall hallucinating after the seizures and admitted to taking a greater dose of baclofen than prescribed for her arthritic joint pain a few hours before experiencing the initial seizure, suggesting a possible predisposition to seizures. Inflammatory markers, including ESR, CRP, and CK, were elevated. Leukocytosis was noted, likely secondary to steroid use. Lactic acid, acetaminophen, and salicylate levels were all within normal limits. Urine drug screen was positive for benzodiazepines, consistent with the patient’s use of alprazolam. HCG was negative. HIV and RPR were non-reactive. Immunologic workup was remarkable for elevated ANA titer, and rheumatoid factor was unexpectedly negative. Head CT, brain MRI and MRA, and EEG were all unremarkable. Throughout her nine-day hospital stay, the patient did not experience another seizure; however, she continued exhibiting visual and auditory hallucinations intermittently and, thus, neurology performed a lumbar puncture and ordered serum autoantibodies suspecting the possibility of autoimmune encephalitis. The patient was started on IVIG while awaiting the results of CSF studies, which were ultimately all negative. However, serum thyroid peroxidase and thyroglobulin antibodies were found to be significantly elevated, confirming the suspicion of an autoimmune etiology. After three days on IVIG, the patient returned to baseline mental status. She was discharged on a five-day course of high-dose oral prednisone and advised to follow up with her primary care physician, neurologist, endocrinologist, and rheumatologist.
Discussion: This case demonstrates that autoimmune encephalitis should be considered among the differential diagnoses in the workup of psychiatric disorders, especially in patients with a history of autoimmunity. Although the pathophysiology of this condition is not fully understood, literature reports successful treatment with immunomodulatory drugs. The outcome of this case aligns with the current literature by demonstrating return to baseline mental status after a three-day course of IVIG followed by five days of high-dose oral corticosteroids.