Abstract
Introduction: Polyclonal gammopathy refers to the overproduction of more than one class of immunoglobulins by plasma cells. Among its many disease associations is human T-lymphotropic virus type 1 (HTLV-I) associated myelopathy (HAM), also known as tropical spastic paraparesis (TSP). HTLV-I is a retrovirus that infects T-lymphocytes and may be transmitted through blood transfusion, sexual contact, during childbirth or breastfeeding. It is endemic to sub-Saharan Africa, South America, Southwest Japan, the Caribbean, and the central region of Australia. We present a case of HAM in the setting of polyclonal gammopathy.
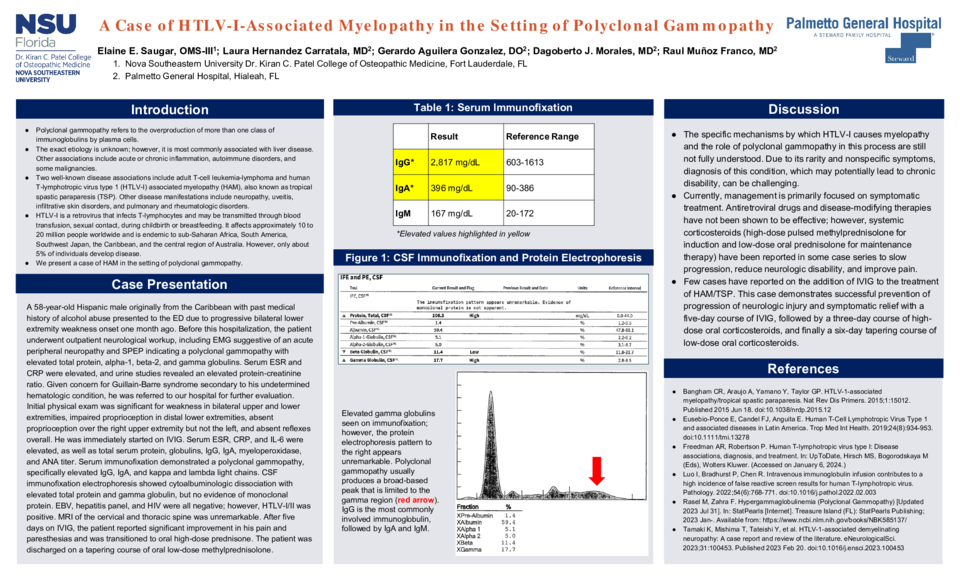
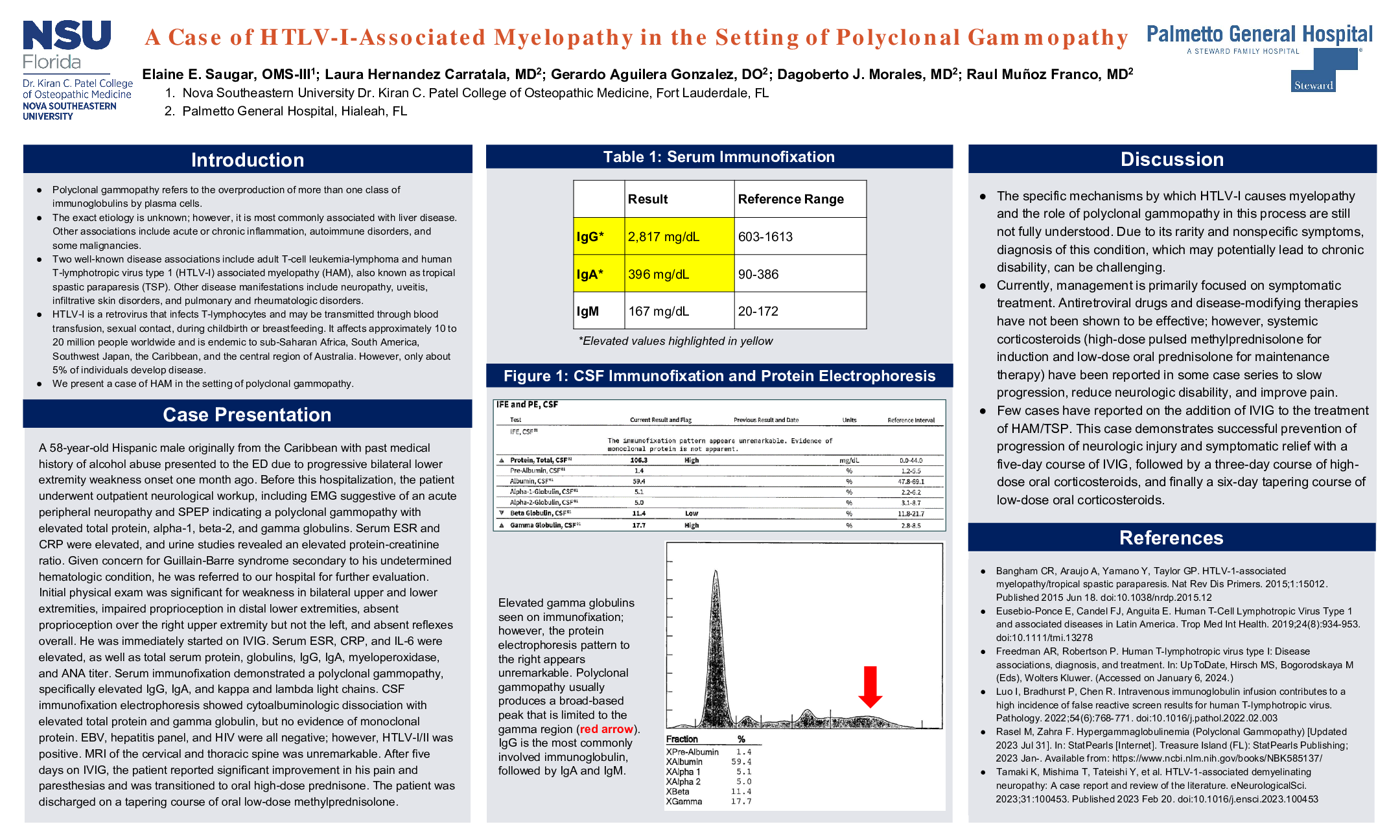
Case Description: A 58-year-old Hispanic male originally from the Caribbean with past medical history of alcohol abuse presented to the ED due to progressive bilateral lower extremity weakness onset one month ago. Three weeks earlier, the patient had been admitted to another hospital for workup; however, no definitive diagnosis was determined. After discharge, he followed up outpatient with a neurologist. EMG was suggestive of an acute peripheral neuropathy. SPEP indicated a polyclonal gammopathy with elevated total protein, alpha-1, beta-2, and gamma globulins. ESR and CRP were elevated, and urine studies revealed an elevated protein-creatinine ratio. Given concern for Guillain-Barre syndrome secondary to his undetermined hematologic condition, he was referred to our hospital for further evaluation. Initial physical exam was significant for weakness in bilateral upper and lower extremities, impaired proprioception in distal lower extremities, absent proprioception over the right upper extremity but not the left, and absent reflexes overall. He was immediately started on IVIG. Inflammatory markers (ESR, CRP, IL-6) were elevated, as well as total serum protein, globulins, IgG, IgA, myeloperoxidase, and ANA titer. Serum immunofixation demonstrated a polyclonal gammopathy, specifically elevated IgG, IgA, and kappa and lambda light chains. Lumbar puncture was performed and CSF analysis only demonstrated elevated herpes I/II IgG and West Nile virus IgG, suggesting previous infection. CSF immunofixation electrophoresis showed cytoalbuminologic dissociation with elevated total protein and gamma globulin, but no evidence of monoclonal protein. EBV, hepatitis panel, and HIV were all negative, but HTLV-I/II was positive. MRI of the cervical and thoracic spine was unremarkable. After five days on IVIG, the patient reported significant improvement in his pain and paresthesias and was transitioned to oral high-dose prednisone. The patient was discharged on a tapering course of oral low-dose methylprednisolone and advised to follow up with neurology, hematology, and his primary care physician.
Discussion: The specific mechanism by which HTLV-1 causes myelopathy and the role of polyclonal gammopathy in this process are not fully understood. Management is focused on symptomatic treatment. Antiretroviral drugs and disease-modifying therapies have not been shown to be effective; however, systemic corticosteroids have been reported in some case series to slow progression, reduce neurologic disability, and improve pain. Few cases have reported on the use of IVIG. This case demonstrates successful prevention of progression of neurologic injury and symptomatic relief with a five-day course of IVIG, followed by a three-day course of high-dose oral corticosteroids, and finally a six-day tapering course of low-dose oral corticosteroids.