Abstract
Introduction: Rural healthcare provider shortages and limited access to skill development and training in rural and remote (R&R) settings pose challenges to healthcare delivery. Simulation-based education (SBE) offers a solution to bridge this gap. This poster discusses the development, testing, and evaluation of a melanoma simulator using additive manufacturing techniques, particularly 3D printing, to enhance the skills of healthcare providers in R&R settings. The simulator was used in a workshop at the 30th Annual Rural and Remote Medicine Course hosted by the Society of Rural Physicians of Canada (SRPC).
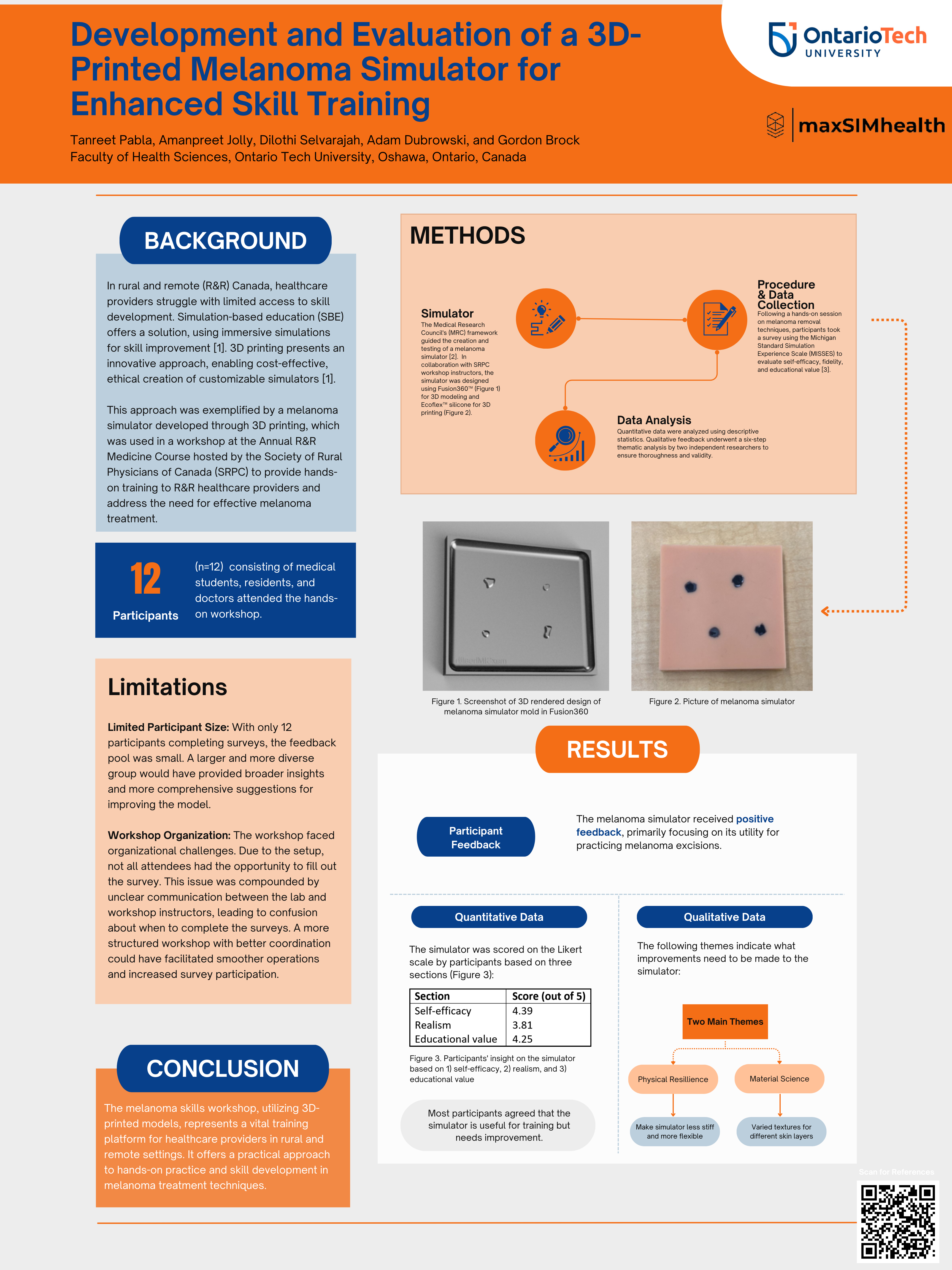
Methods: This study applies the Medical Research Council's (MRC) framework, adapting it to develop, test, and pilot a melanoma simulator. This structured approach, emphasizes practicality, acceptability, and effectiveness in designing and evaluating complex medical education simulators. Feedback from learners and instructors is integral for refining the simulator's design. In collaboration with SRPC workshop instructors, the melanoma simulator was designed using Fusion360™ to feature various melanomas in shapes and depths. Produced with 3D printing and Ecoflex™ silicone, each simulator costs $12.00 CAD, mimicking real skin tones and melanoma characteristics. Twelve medical students, residents, and doctors attended the workshop, consenting to data usage in future publications. Held in a conference room, the workshop involved practical melanoma removal techniques using the simulator, with participants receiving direct instruction and feedback from experts. Post-workshop, they completed a paper-based survey based on the Michigan Standard Simulation Experience Scale (MISSES), covering self-efficacy, realism, and educational value. The survey included a 5-point Likert scale and open-ended questions, with participants informed about the study's procedures and giving their consent. Quantitative data, including means and standard deviations, were employed for analysis, while qualitative data underwent independent analysis by two researchers using a six-step procedure to identify and refine themes, ensuring analysis validity.
Results: The melanoma simulator received positive feedback for its utility in practicing melanoma excisions. Participants rated their confidence highly (4.39/5) but had concerns about realism (3.81/5), although they found it effective for learning (4.25/5). Most participants agreed the simulator is useful for training but needs improvement. Qualitatively, two main themes emerged: Physical Resilience - participants suggested making the simulator more flexible; Material Science - feedback included the need for varied textures and appreciation for diverse skin tones. Suggestions for improvement focused on enhancing physical resilience and material properties to increase realism and functionality.
Discussion: Limitations, including a small participant sample and workshop organization issues, are discussed. Despite limitations, the study demonstrates the potential of 3D-printed simulators to provide cost-effective and ethical training opportunities for R&R healthcare providers.
Conclusion: The study underscores the importance of practical training opportunities for R&R healthcare providers and highlights the efficacy of 3D-printed simulators in addressing skill development challenges in rural settings.