Abstract
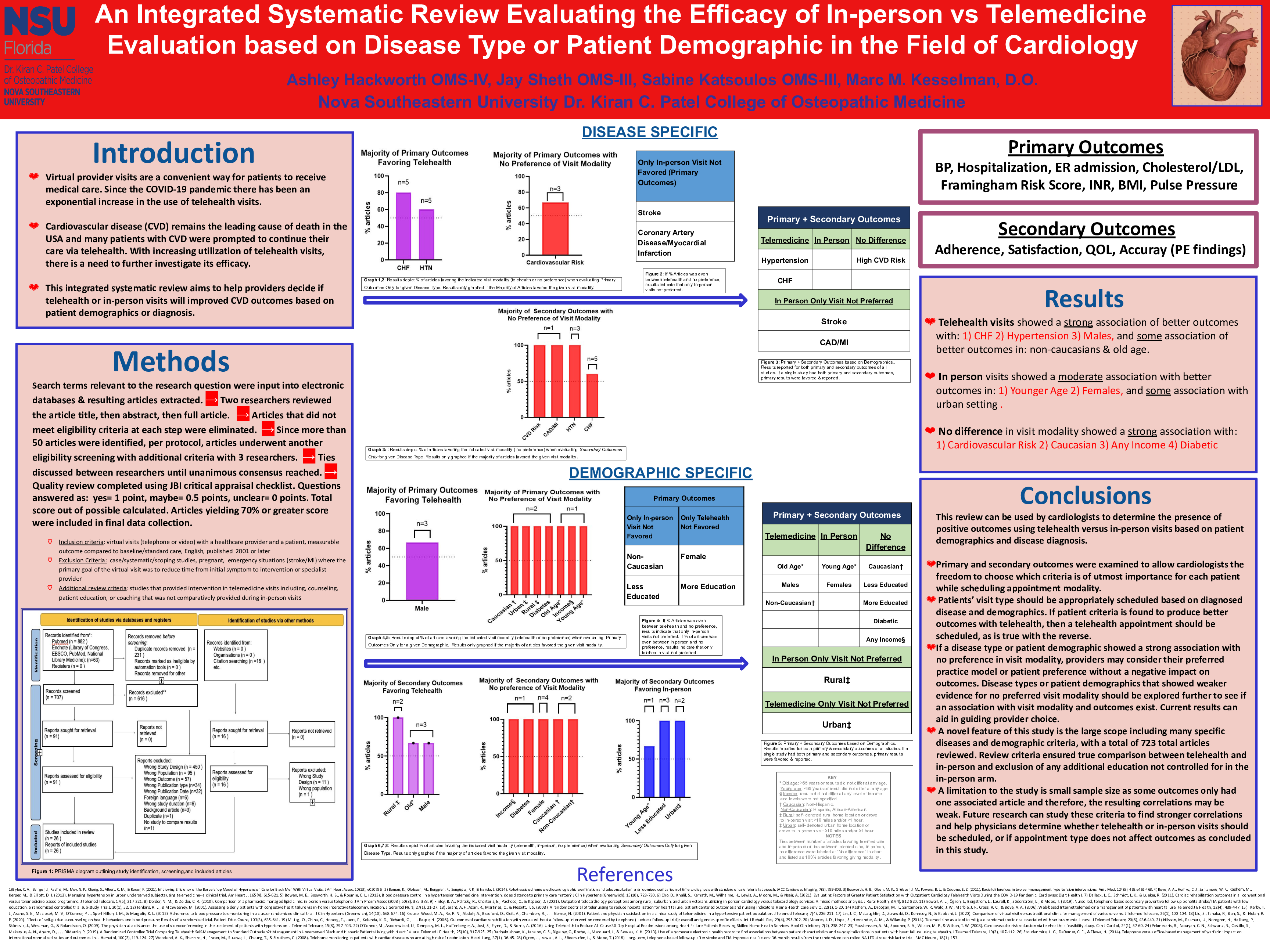
Background: In 2019, cardiovascular disease was the most common cause of death in the USA. Also, since the COVID-19 pandemic, there has been a significant increase in the number of virtual provider visits. Therefore, there is a growing need to evaluate the efficacy of telemedicine versus usual care in the field of cardiology. This study aims to help providers decide which visit type will result in improved cardiovascular outcomes based on patients’ specific characteristics.
Objective : To determine if cardiovascular outcomes improved more with in-person provider visit, a telemedicine visit (virtual), or either visit type based on cardiovascular disease types, risk factors, intervention, or patient demographics.
Methods: The study is an integrated systematic review and articles were retrieved from PubMed. Articles included met the following criteria: a study with a virtual visit (telephone or video based) with a healthcare provider and human patient, written in English, and published in 2001 or later. Articles were excluded if they met the following criteria: remote patient monitoring only studies, case studies, systematic reviews, scoping reviews, emergency situations (stroke/myocardial infarction) where the primary goal of the virtual visit was to reduce the time from initial symptom onset to intervention or specialist provider, or studies that provided intervention in telemedicine visits including, counseling, patient education, or coaching that was not comparatively provided during in-person visits.
Results: Of the 707 articles reviewed, 681 were excluded, and 26 articles were examined. The majority of articles found that cardiovascular outcomes improved more during telemedicine visits if the patient had any of the following characteristics: Hypertension diagnosis, Congestive Heart Failure (CHF) diagnosis, male gender, non-Caucasian, or older age (>65 years old). The majority of articles found that cardiovascular outcomes improved more with in-person visits if the patient had any of the following characteristics: younger age (<65 years old), female, or lived in an urban setting. The majority of articles found that cardiovascular outcomes did not differ significantly whether the visit was performed in person or via telemedicine, especially if the patient had the following characteristics: cardiovascular risk, Caucasian, any income level, or diabetic.
Conclusions: The majority of cardiovascular disease types or patient characteristics did not show a difference in improved outcomes based on visit type. Therefore, patient and provider preferences can be taken into account when choosing between an in-person or telemedicine visit for most cardiovascular patients. Patients who are younger age (<65 years old), females, or live in an urban setting may be better suited to an in-person visit. Alternatively, patients who are male, have congestive heart failure, have hypertension, identify as non-Caucasian, or who are of older age (>65 years old) may have more favorable cardiovascular outcomes if seen at a telemedicine visit.