Abstract
Purpose
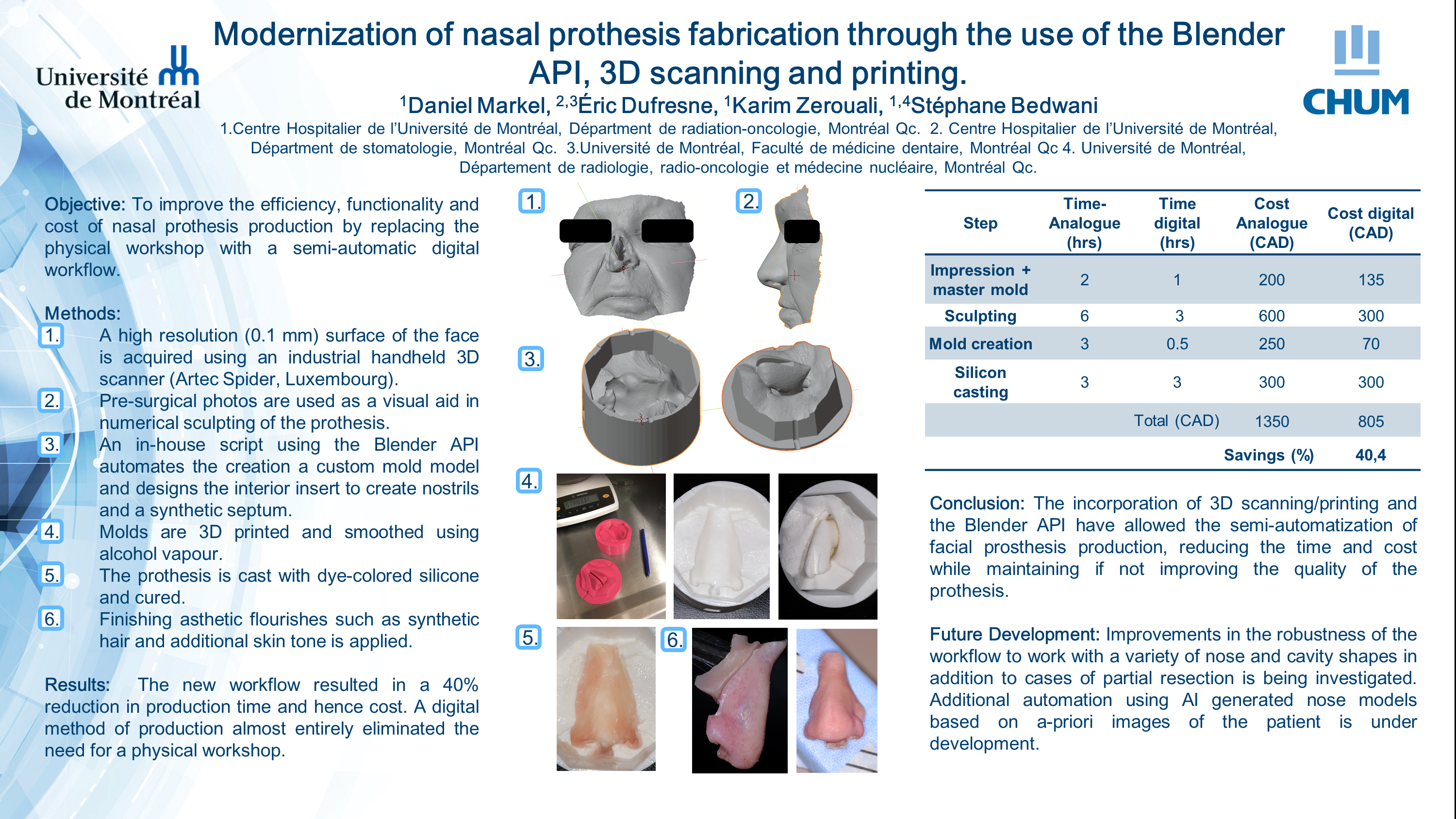
To improve the efficiency, functionality and cost of nasal prosthesis production for cancer patients who have received a full or partial surgical resection of the nose. The main objective of this work is to digitize the entire workflow for nasal prosthesis creation by incorporating automation, 3D scanning and printing.
Materials and Methods
An industrial handheld 3D scanner (Artec, Luxembourg) is used to provide high resolution facial scans (0.1 mm) of the patient, specifically the nasal cavity and surrounding area. This has the advantage of minimizing geometric distortions compared to an analogue casting process. Using Zbrush (Pixologic, Los Angeles, CA, USA), the nose is sculpted digitally in 3D with the assistance of photographs taken prior to the surgery. Using the nose model and facial scan, an in-house Python script using the Blender API (Blender Foundation, Amsterdam, The Netherlands) fully automates the creation of a mold using a series of morphological procedures and rules. This includes the generation of both male and female pieces along with an insert to maintain breathing channels and a synthetic septum in order to mimic the functionality and feel of a real nose. The molds are then 3D printed and filled with silicon mixed with dyes in order to match the patients’ skin tone. Additional aesthetic flourishes are then added manually such as the addition of synthetic hair and dyes to create a realistic texture.
Results
The new workflow is able to reduce the nasal prosthesis production time from a manually intensive 2 days to 6 hours excluding printing time. This time and material savings between the two processes translates to an approximate cost reduction of $545 per prosthetic or 40% of the conventional cost of production. As of this writing, 4 patients have had prostheses created from the new semi-automatic pipeline.
Conclusions
The incorporation of 3D scanning/printing and the Blender API have allowed the semi-automatization of facial prosthesis production, reducing the time and cost while maintaining if not improving the quality of the prothesis. Digitization of the process improves fidelity compared to analogue plaster molds and allows molds and the prosthesis to be easily reprinted and recast at a future date, which is not always possible with plaster molds should they become damaged over time. Some challenges remain to fully account for the variability of patient morphology which can cause failures in the mold generation script.