Abstract
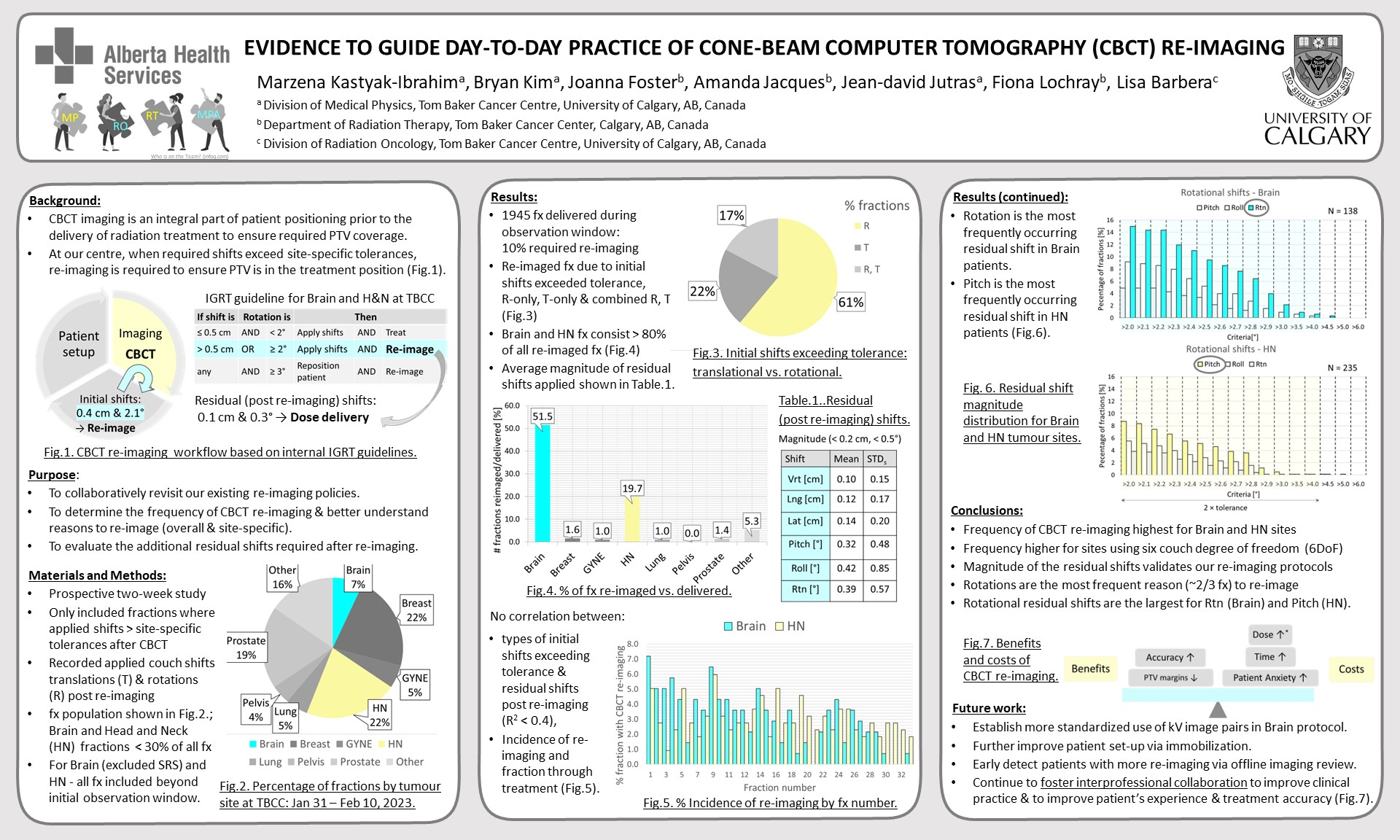
PURPOSE: Cone-beam Computer Tomography (CBCT) imaging is an integral part of patient positioning prior to the delivery of radiation treatment. At our institution, when shifts applied from initial CBCT exceed the set tolerance specific to each tumour site, CBCT is repeated to ensure that the target is in the planned position. There are both benefits and costs associated with CBCT reimaging which directly impacts day-to-day clinical practice. A better understanding of the need to re-image is of interest to all professionals involved in the patient treatment. This study is part of a larger project aimed at evaluating our existing clinical practice of re-imaging, the reasons for re-imaging and determining the cases where the benefit of re-imaging is evident. The purpose of this preliminary study was to determine the frequency of CBCT re-imaging as dictated by site-specific protocols used in the clinic and to evaluate whether additional shifts were still required after re-imaging.
MATERIALS AND METHODS: This is a prospective cross-sectional study. Over a two-week period, every patient requiring repeat CBCT was captured manually. We only included re-imaging cases where applied shifts exceeded our institutional tolerances for translational and rotational corrections. Repeat imaging related to bowel and bladder issues, as well as other set-up issues were excluded. Information collected included magnitude of couch shifts and rotations applied after CBCT re-imaging as well as tumor group.
RESULTS: 1945 fractions were delivered during the two-week observation window. Of these over 10% required re-imaging. More than 80% of the fractions during which re-imaging occurred were from patients with head and neck and brain cancer (the distribution between the two groups was even; the brain group did not include stereotactic radiosurgery patients). Almost two-thirds of re-imaging cases resulted from rotational corrections exceeding tolerance, while 21% and 16% of cases were due to the translation only corrections and translational combined with rotational corrections, respectively. On average, the absolute value of all the translational shifts (vertical, longitudinal, and latitudinal) applied after re-imaging was smaller than 0.2 cm and rotations shifts (Pitch, Roll, and Rotation) were smaller than 0.5°.
CONCLUSIONS: We conclude that CBCT re-imaging is common, seen most often in patients with head and neck or brain cancer. This preliminary work will lead to site-specific evaluations starting with brain and head and neck to find ways to further improve our clinical practice, while fostering interprofessional collaboration.