Abstract
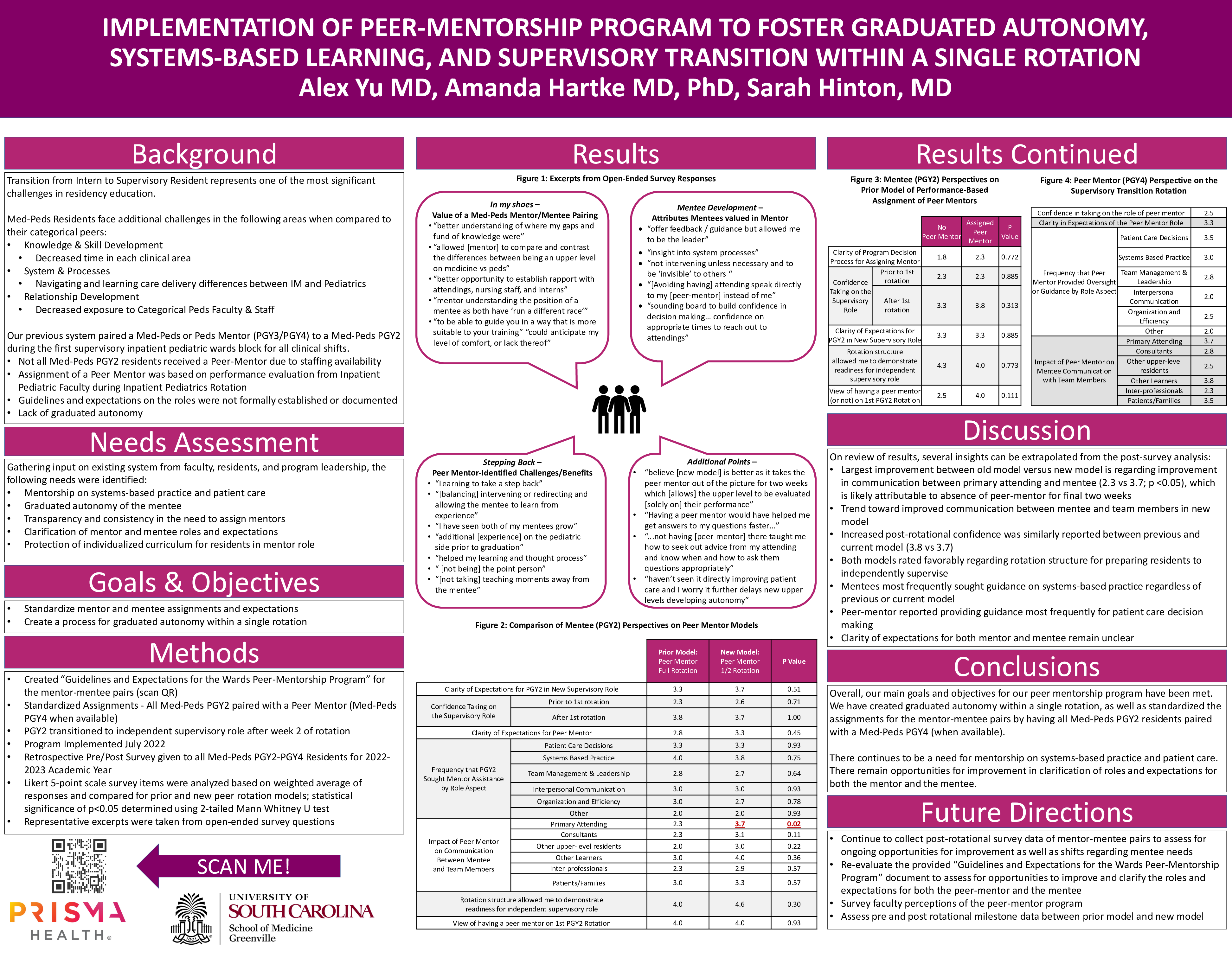
Medicine-Pediatrics curriculum is built to train residents into highly competent dual-trained physicians but limited exposure in some clinical areas prior to transitioning to a supervisory resident role can lead some residents to feel underprepared for this role. As an approach to these concerns, our institution previously utilized a system where a more senior resident advised and monitored new PGY2s throughout their first Inpatient Pediatrics supervisory rotation. However, this system lacked uniformity and raised concerns about increasing learner performance anxiety and difficulty assessing the PGY2’s performance. To address these concerns, we created and implemented an innovative Peer-Mentorship Program with the goal of fostering graduated autonomy, systems-based learning, and supervisory transition within a single rotation. In brief, this program pairs all Med-Peds PGY-2 residents with a Med-Peds PGY4 peer mentor during the first 2 weeks of the PGY-2’s first Inpatient Pediatrics supervisory month. To assess the outcomes of the implemented program, qualitative and quantitative data were obtained from an anonymous resident survey including both Likert and open-ended questions as well as de-identified evaluation data. Likert 5-point scale survey items were analyzed based on weighted average of responses and compared for prior and new peer rotation models; statistical significance of p<0.05 determined using 2-tailed Mann Whitney U test. On review of results, the largest improvement between old model versus the new model of the peer mentorship program was noted in the area of communication between primary attending and mentee (2.3 vs 3.7; p<0.05), which is likely attributable to absence of peer-mentor for final two weeks. There was a trend toward improved communication between mentee and team members in new model. In regard to post-rotational confidence, this was rated similarly between old model versus new model (3.8 vs 3.7). Both models rated favorably regarding rotation structure for preparing residents to independently supervise. Mentees reported seeking peer-mentor guidance most frequently on systems-based practice issues in both models. Peer mentors reported providing guidance most frequently for patient care decision making. The clarity of role expectations for both mentor and mentee remained unclear. Overall, our main goals and objectives for our peer mentorship program have been met. We have created graduated autonomy within a single rotation, as well as standardized the assignments for the mentor-mentee pairs by having all Med-Peds PGY2 residents paired with a Med-Peds PGY4 (when available). There continues to be a need for mentorship on systems-based practice and patient care. There remain opportunities for improvement in clarification of roles and expectations for both the mentor and the mentee.