Abstract
Purpose: Working at a cancer centre can be immensely rewarding, yet it is also highly demanding and associated with significant stressors. Therefore, it is important to develop approaches that will make it easier for oncology healthcare professionals to feel more satisfied with their work experience and allow them to provide the best care possible.
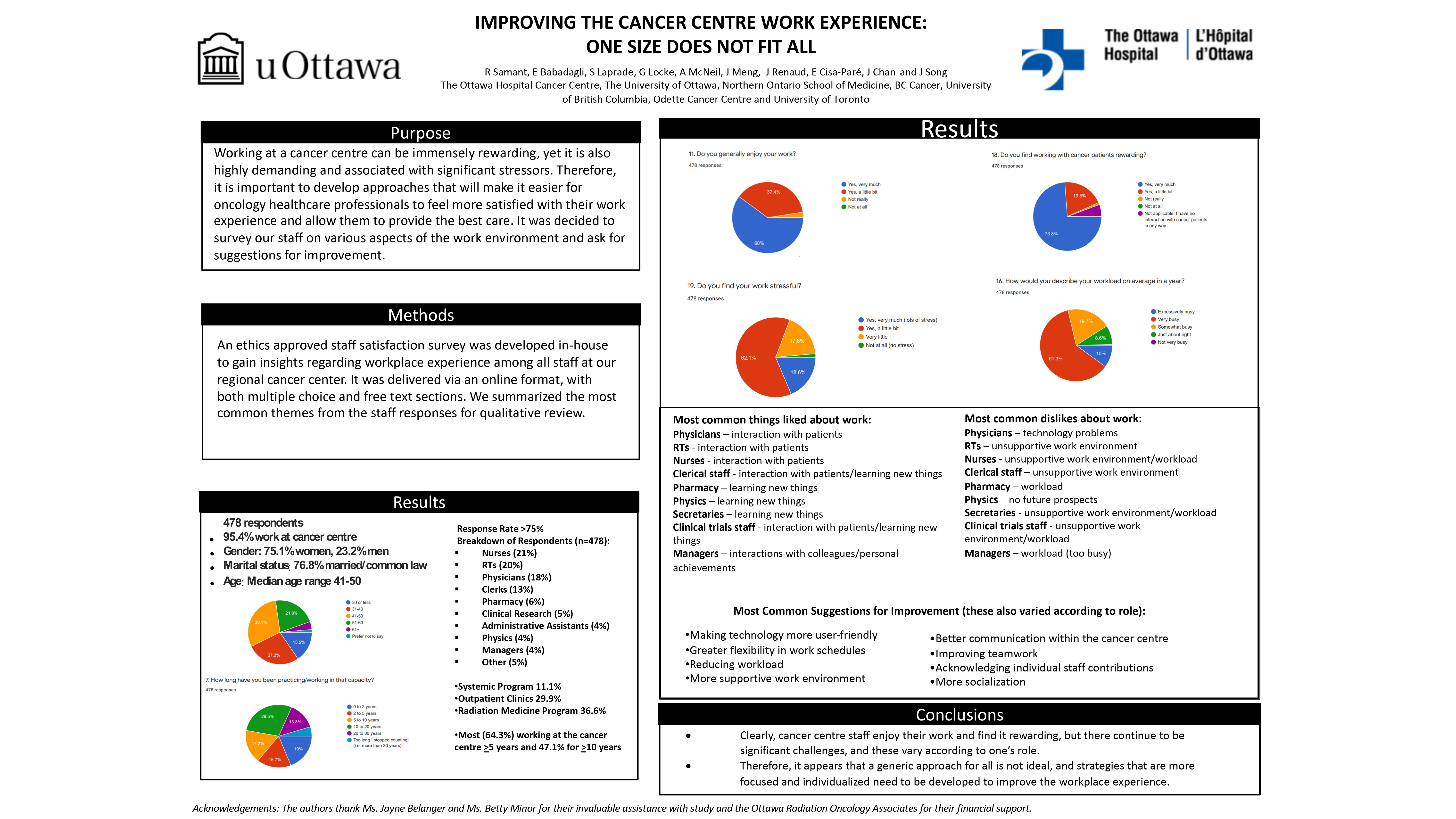
Methods: An ethics approved staff satisfaction survey was developed in-house to gain insights regarding workplace experience among all staff at our regional cancer center. It was delivered via an online format, with both multiple choice and free text sections. We summarized the most common themes from the staff responses for qualitative review.
Results: In total, 478 individuals completed the online survey. This represented the majority of the cancer centre staff, with 75.1% women, 23.2% men and 1.7% preferring not to say. The median age range was 41-50 years, with 76.8% either married or in common-law relationships. Most (64.3%) had worked at the cancer center for at least 5 years, with almost half (47.1%) having worked for 10 or more years. The breakdown according to healthcare professional type was as follows: 21% nurses, 20% radiation therapists, 18% physicians, 13% clerical staff, 6% pharmacy, 5% clinical research, 4% administrative assistants, 4% physics, 4% managers and 5% other types of staff. Almost all (97.4%) generally enjoyed their work and found working with cancer patients rewarding (93.3%). There was definite evidence of work-related stress; 18.6% stated it was “very much” and 62.1% “a little bit”. In terms of their workload, 61.3% stated it was "very busy" and 10% stated it was "excessively busy”. The dislikes and workplace challenges varied according to staff role and the most common ones were as follows: unsupportive work environment for radiation therapists and clerical staff; technology problems for physicians; excessive workload for pharmacy and managers; no future prospects for physics; and a combination of unsupportive work environment and workload for nurses, clinical trials staff and administrative assistants. Similarly, suggestions for improvement also varied depending on staff role and included the following: making technology more user-friendly, greater flexibility in work schedules, reducing workload, more supportive work environment, better communication within the cancer centre, improving teamwork and acknowledging individual staff contributions.
Conclusions: Clearly, cancer centre staff enjoy their work and find it rewarding, but there continue to be significant challenges, and these vary according to one’s role. Therefore, it appears that a generic approach for all is not ideal, and strategies that are more focused and individualized need to be developed to improve the workplace experience.