Abstract
Introduction: Peripheral artery disease (PAD) affects approximately 7% of adults in the U.S., and it occurs more frequently in patients with a history of tobacco use, hypertension, diabetes, and hypercholesterolemia. These risk factors can lead to the most common cause of PAD: atherosclerosis. However, additional causes that may not be suspected initially include fibromuscular dysplasia, vasculitis, and radiation-induced atherosclerosis. The patient described in this article had 36 radiation therapies directly to the pelvis and bladder due to bladder cancer. The damage caused by radiation therapy to the heart and coronary arteries is well-established in the literature; however, radiation as a cause of PAD has not been as extensively investigated.
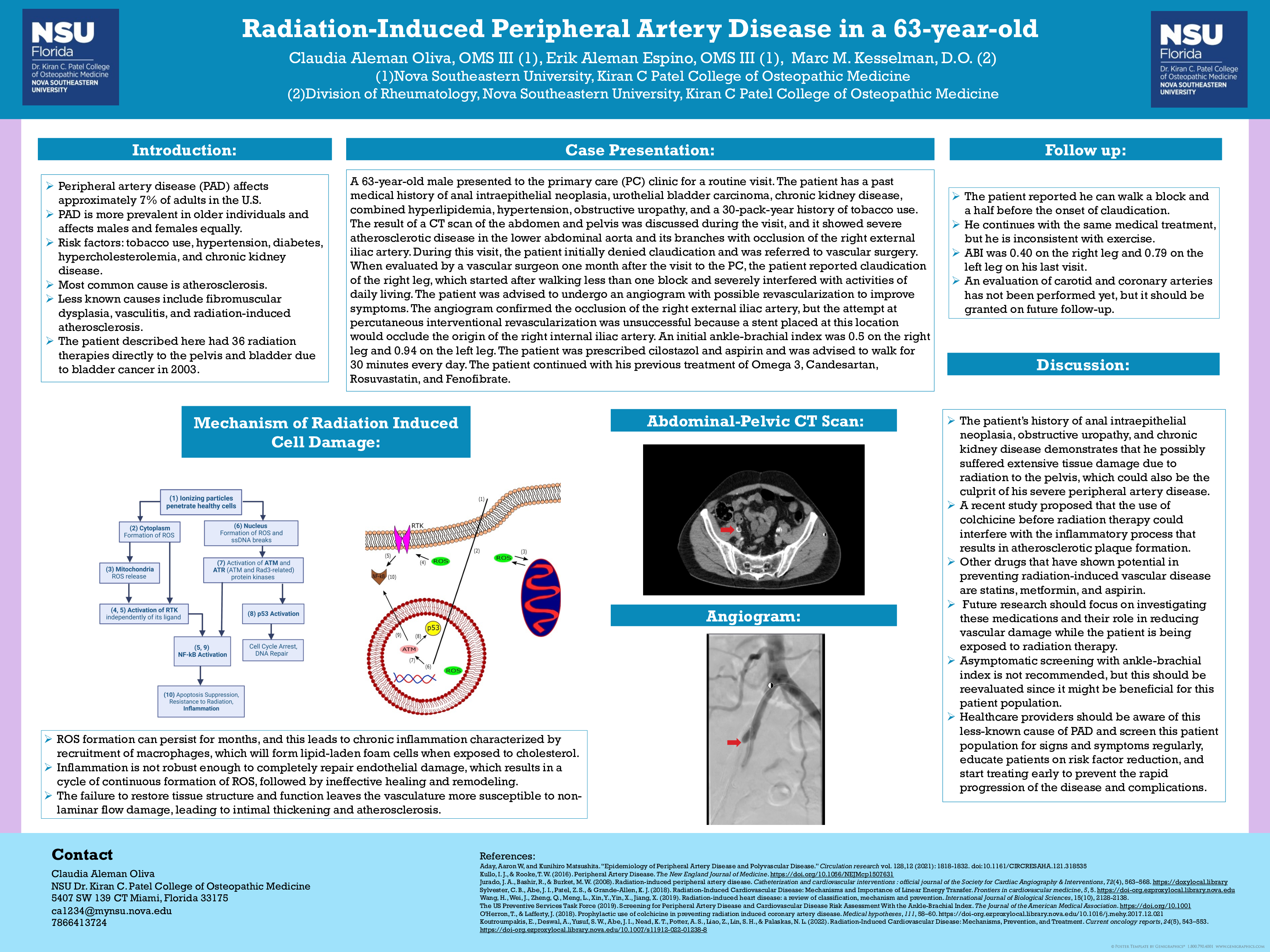
Case Description: A 63-year-old male presents to the primary care (PC) clinic for a routine visit. The patient has a past medical history of anal intraepithelial neoplasia, urothelial bladder carcinoma, chronic kidney disease, combined hyperlipidemia, hypertension, obstructive uropathy, and a 30-pack-year history of tobacco use. The result of a CT scan of the abdomen and pelvis was discussed during the visit, and it showed severe atherosclerotic disease in the lower abdominal aorta and its branches with occlusion of the right external iliac artery. During this visit, the patient initially denied claudication and was referred to vascular surgery. When evaluated by a vascular surgeon one month after the visit to the PC, the patient reported claudication of the right leg, which started after walking less than one block and severely interfered with activities of daily living. The patient was advised to undergo an angiogram with possible revascularization to improve symptoms. The angiogram confirmed the occlusion of the right external iliac artery, but the attempt at percutaneous interventional revascularization was unsuccessful because a stent placed at this location would occlude the origin of the right internal iliac artery. The patient was prescribed cilostazol and aspirin and was advised to walk for 30 minutes every day. On follow-up, the patient reported symptomatic improvement.
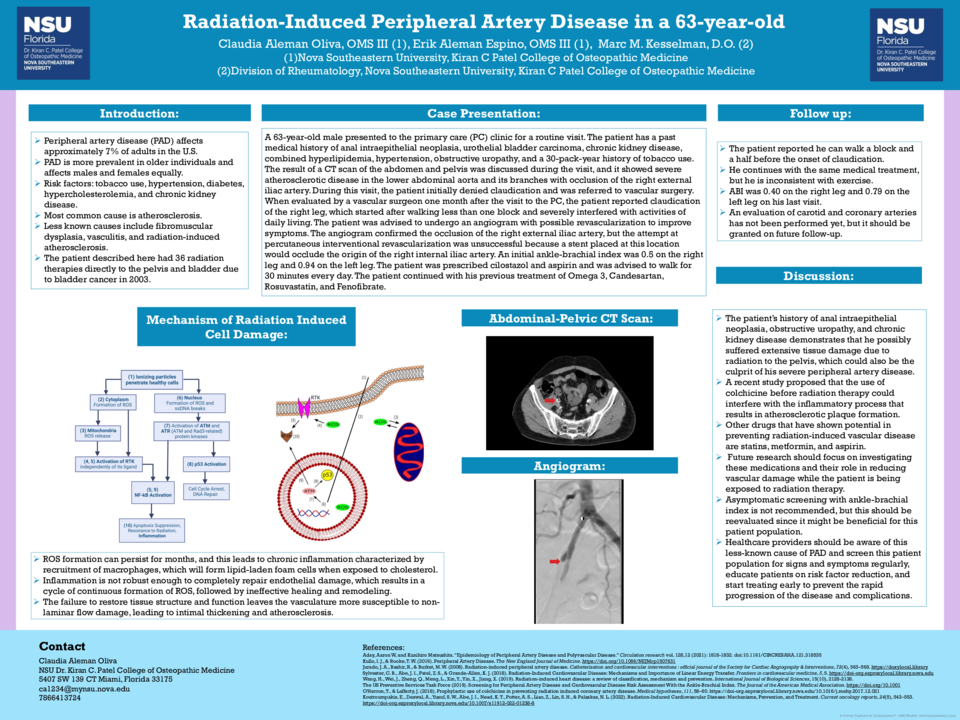
Discussion: The presence of severe peripheral artery disease on this patient's right external iliac artery, the same area where he received radiation therapy, raises the question of whether atherosclerosis might have been caused by radiation therapy. Additionally, his history of anal intraepithelial neoplasia, obstructive uropathy, and chronic kidney disease further demonstrates that he possibly suffered extensive tissue damage due to radiation to the pelvis. Healthcare providers should be aware of this less-known cause of peripheral artery disease to prevent complications through the reduction of risk factors and early symptomatic screening. Currently, asymptomatic screening with ankle-brachial index is not recommended, but this should be reevaluated since it might be beneficial for this patient population. Future research should focus on finding preventive treatments that reduce vascular damage while the patient is being exposed to radiation therapy.