Abstract
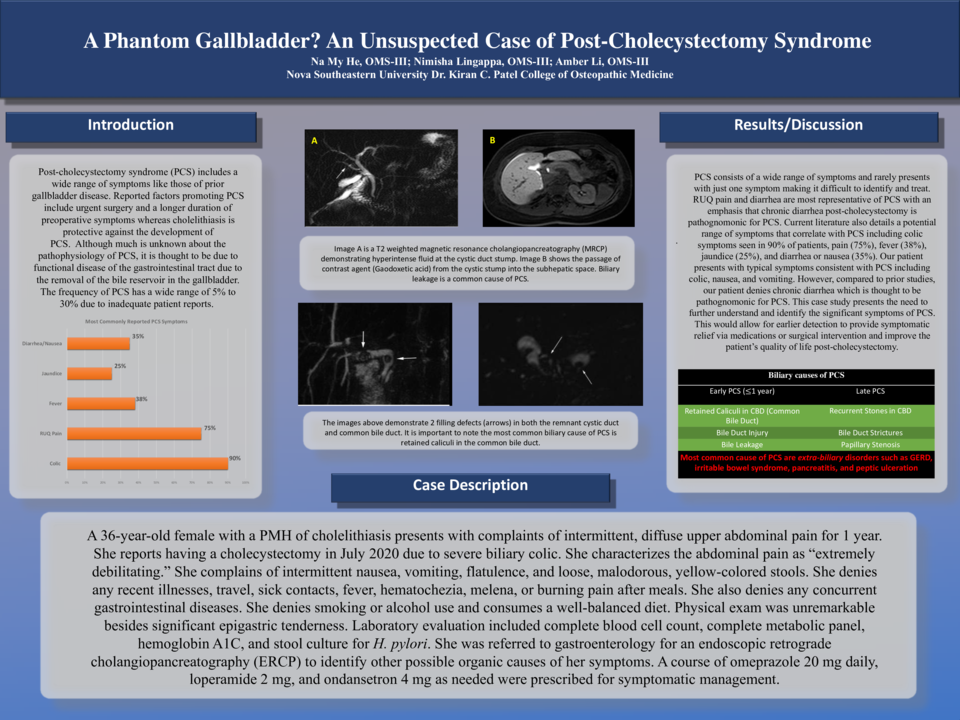
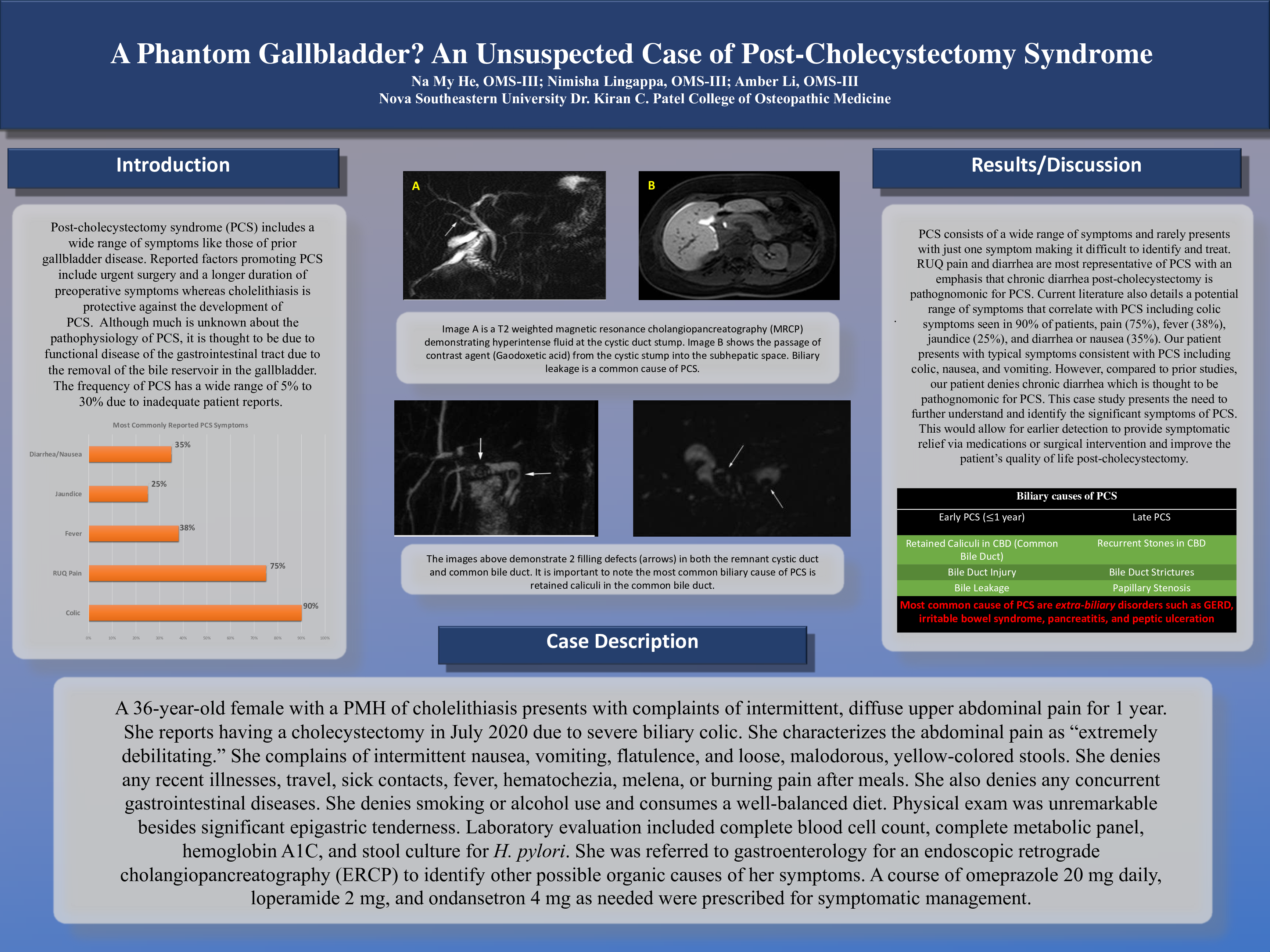
Post cholecystectomy syndrome (PCS) includes a wide range of symptoms like those of prior gallbladder disease. PCS consists of a wide range of symptoms and seldom presents with only one symptom thus making PCS difficult to identify and treat. RUQ pain and diarrhea are most commonly representative of PCS with an emphasis that chronic diarrhea after cholecystectomy is pathognomonic for postoperative pain. Current literature also details a potential range of symptoms that correlate with PCS including colic symptoms as seen in 90% of patients, pain (75%), fever (38%), jaundice (25%), and diarrhea or nausea (35%).
The pathophysiology of PCS, it is thought to be due to functional disease of the gastrointestinal tract due to the removal of the bile reservoir in the gallbladder. The frequency of PCS has a wide range of 5% to 30% due to inadequate patient reports. Hence, the diagnosis of PCS is often overlooked and underdiagnosed due to non-specific manifestations that can easily be attributed to other gastrointestinal diseases or illnesses.
In our case study, our patient presents with atypical symptoms inconsistent with those commonly associated with PCS and denies fever, jaundice, RUQ pain, and diarrhea. Instead, the patient complains of diffuse abdominal pain, intermittent nausea, and loose stools with no past medical history of gastrointestinal disease besides cholelithiasis. Compared to prior studies, this patient denies chronic diarrhea which is thought to be pathognomonic for severe PCS pain. This case study presents the need to further understand and identify the significant symptoms of PCS for earlier detection to provide symptomatic relief via medications or surgical intervention to improve the patient’s quality of life post-cholecystectomy.