Abstract
Introduction: Central nervous system (CNS) vasculitis is a rare complication of corona virus disease (COVID-19), characterized by inflammation and damage to blood vessels in the brain and spinal cord. While the virus is primarily known for its respiratory symptoms, it has been found to affect multiple organ systems, including the nervous system. The mechanisms by which COVID-19 leads to CNS vasculitis are not yet fully understood, but it is thought that the virus may directly or indirectly affect the blood-brain barrier, leading to inflammation and damage to the blood vessels. The purpose of this paper is to present a case of CNS vasculitis in a corona virus disease (COVID-19) patient and discuss diagnostic and therapeutic considerations.
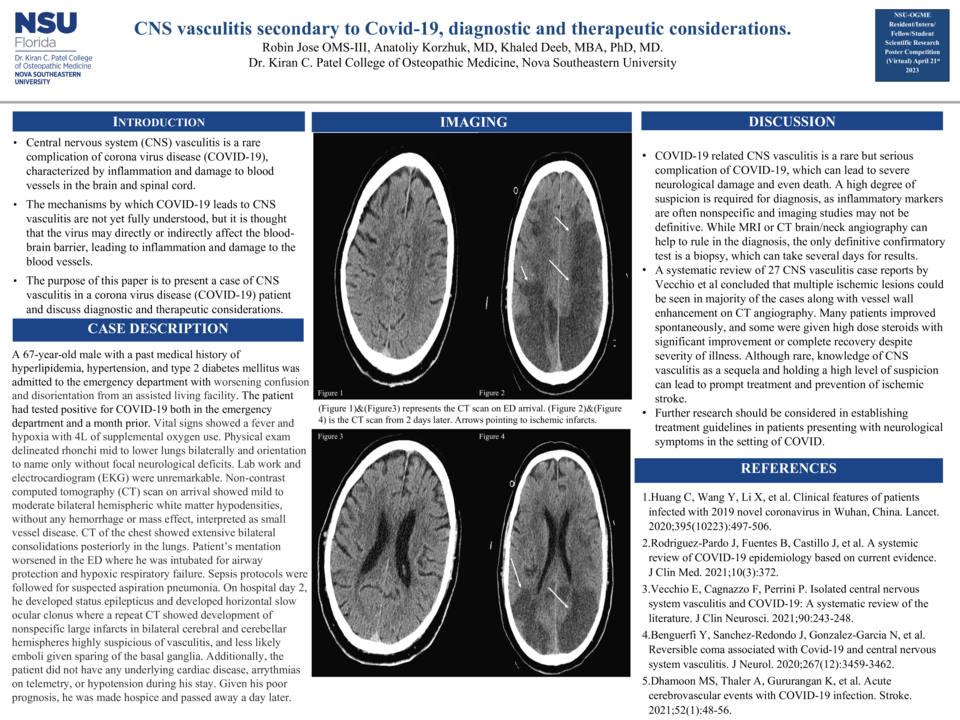
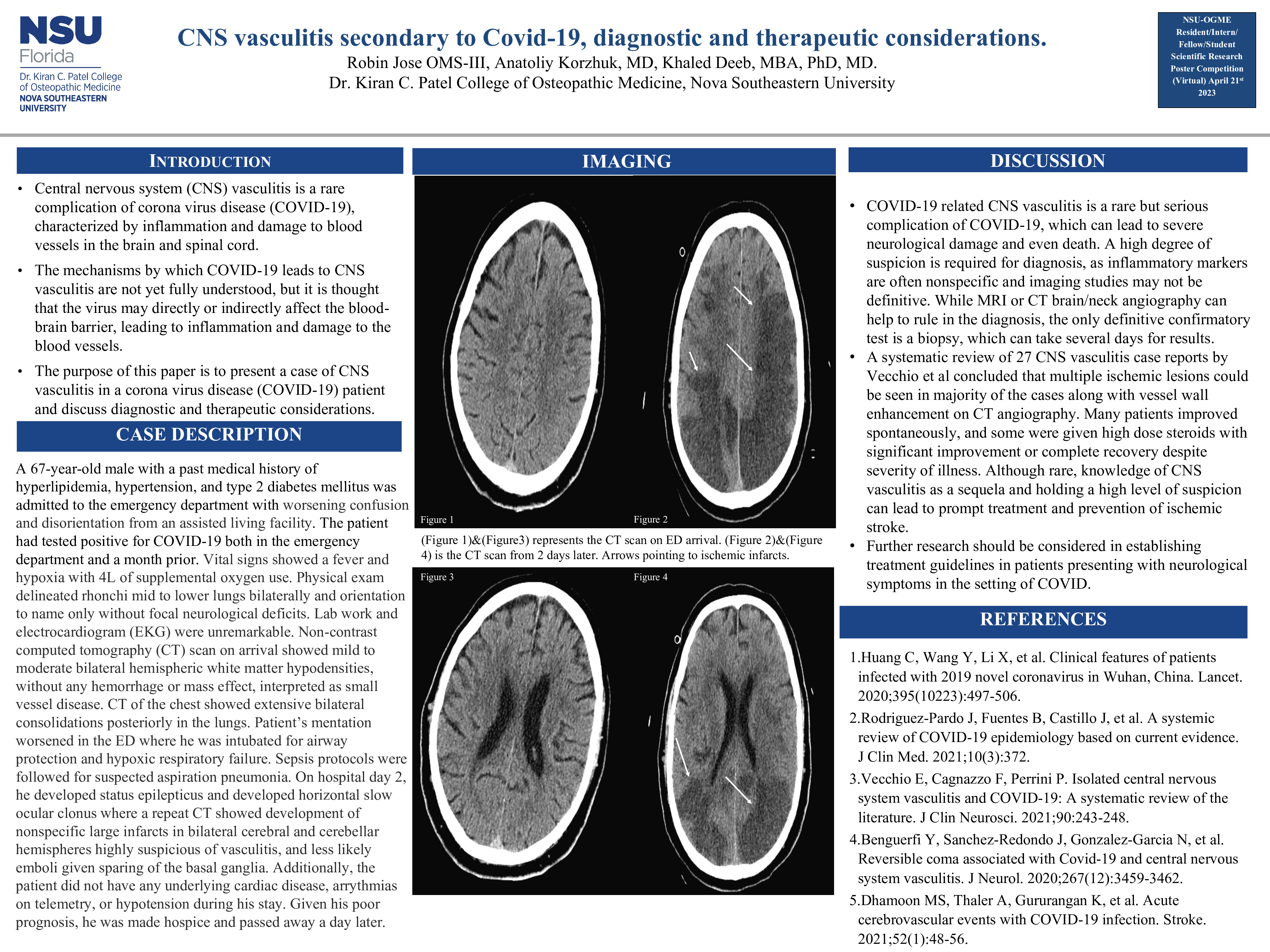
Case Presentation: A 67-year-old male with a past medical history of hyperlipidemia, hypertension, and type 2 diabetes mellitus was admitted to the emergency department with worsening confusion and disorientation from an assisted living facility. The patient had tested positive for COVID-19 both in the emergency department and a month prior. Vital signs showed a fever and hypoxia with 4L of supplemental oxygen use. Physical exam delineated rhonchi mid to lower lungs bilaterally and orientation to name only without focal neurological deficits. Lab work and electrocardiogram (EKG) were unremarkable. Non-contrast computed tomography (CT) scan on arrival showed mild to moderate bilateral hemispheric white matter hypodensities, without any hemorrhage or mass effect, interpreted as small vessel disease. CT of the chest showed extensive bilateral consolidations posteriorly in the lungs. Patient’s mentation worsened in the ED where he was intubated for airway protection and hypoxic respiratory failure. Sepsis protocols were followed for suspected aspiration pneumonia. On hospital day 2, he developed status epilepticus and developed horizontal slow ocular clonus where a repeat CT showed development of nonspecific large infarcts in bilateral cerebral and cerebellar hemispheres highly suspicious of vasculitis, and less likely emboli given sparing of the basal ganglia. Additionally, the patient did not have any underlying cardiac disease, arrythmias on telemetry, or hypotension during his stay. Given his poor prognosis, he was made hospice and passed away a day later.
Discussion: COVID-19 related CNS vasculitis is a rare but serious complication of COVID-19, which can lead to severe neurological damage and even death. A high degree of suspicion is required for diagnosis, as inflammatory markers are often nonspecific and imaging studies may not be definitive. While MRI or CT brain/neck angiography can help to rule in the diagnosis, the only definitive confirmatory test is a biopsy, which can take several days for results. A systematic review of 27 CNS vasculitis case reports by Vecchio et al concluded that multiple ischemic lesions could be seen in majority of the cases along with vessel wall enhancement on CT angiography. Many patients improved spontaneously, and some were given high dose steroids with significant improvement or complete recovery despite severity of illness. Although rare, knowledge of CNS vasculitis as a sequela and holding a high level of suspicion can lead to prompt treatment and prevention of ischemic stroke. Further research should be considered in establishing treatment guidelines in patients presenting with neurological symptoms in the setting of COVID.