Abstract
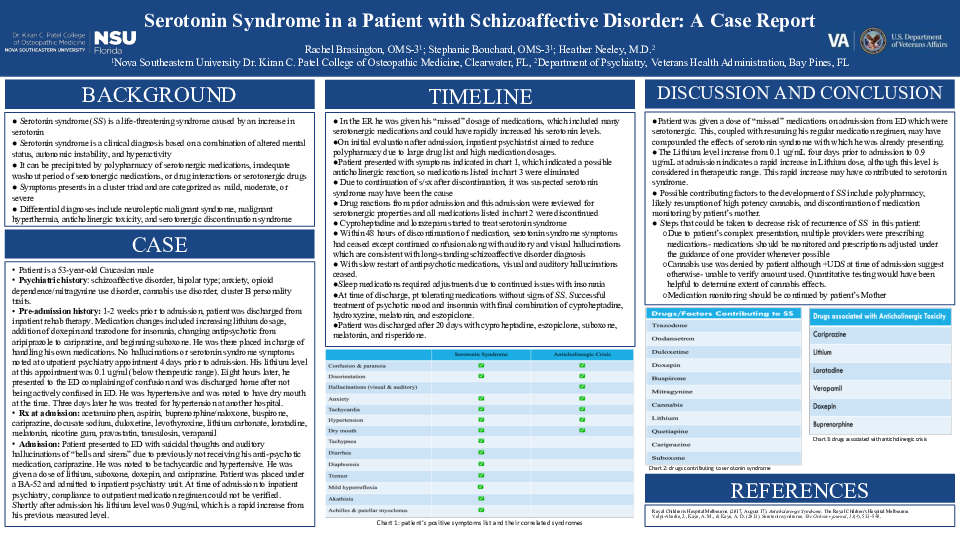
Introduction: Serotonin Syndrome is a possibly life-threatening syndrome caused by an increase in serotonin levels in the body. The prevalence of serotonin syndrome is largely unknown due to the wide array of symptoms and the lack of confirmatory testing. Diagnosis must be made clinically based on a combination of altered mental status, autonomic instability, and hyperactivity. Most cases of serotonin syndrome are precipitated by polypharmacy of serotonergic medications. The list of medications that could play a role is extensive. Diagnosis is made increasingly difficult by the overlapping differential diagnoses such as neuroleptic malignant syndrome, malignant hyperthermia, and anticholinergic toxicity.
Case Description: We present the case of a 53-year-old male with a history of schizoaffective disorder, bipolar type; anxiety, opioid dependence, and cluster B personality traits. Two weeks prior to admission to psychiatric unit, the patient was discharged from an inpatient rehabilitation therapy program. At this program multiple changes were made to the patient’s medication list, and he was put in charge of handling his own medications.
One week after discharge from rehabilitation program, he presented to the ED with complaints of confusion and was found to have dry mouth and hypertension but was not admitted. Three days later, he was treated for hypertension at a different hospital.
The patient was admitted to the psychiatric hospital due to suicidal thoughts and auditory hallucinations. He was tachycardic and hypertensive. The patient was placed under a BA-52 and given lithium, suboxone, doxepin and cariprazine. Outpatient medication regimen and adherence could not be verified.
Due to patient presenting with confusion, paranoia, disorientation, hallucinations, tachycardia, dry mouth, and hypertension, it was initially suspected that he was in an anticholinergic crisis and all anticholinergic medication was discontinued. Due to continuation of symptoms after elimination, serotonin syndrome was suspected. Serotonin containing medications were discontinued and cyproheptadine and lorazepam were initiated. Within 48 hours of discontinuation, all symptoms resolved except the auditory and visual hallucinations. These are consistent with the previous diagnosis of schizoaffective disorder. Gradual restart of antipsychotic medications caused hallucinations to cease.
At time of discharge, patient was tolerating medications without signs of serotonin syndrome with cessation of hallucinations.
Discussion: This case illustrates the importance of clinical history in successfully diagnosing and differentiating serotonin syndrome from other possible differentials.