Abstract
Introduction: Community acquired pneumonia (CAP) and pyelonephritis are common infections that are treated in outpatient settings. CAP is an infection of the lung parenchyma that is usually due to Streptococcus pneumoniae. CAP is diagnosed by the presence of lobar infiltrates on chest imaging and clinical symptoms (including fever, cough, and dyspnea). Pyelonephritis is an acute infection of the kidneys that results from an ascending lower urinary tract infection. The main causative agent in pyelonephritis is Escherichia coli. A urinalysis and symptoms (including fever, dysuria, and flank pain) are used to diagnose patients with pyelonephritis. Imaging for pyelonephritis may be done in severe cases or when the patient does not improve with treatment. CAP and pyelonephritis commonly resolve with empiric treatment consisting of antibiotics. Although community acquired pneumonia and pyelonephritis are common infections in the community, they typically do not coincide or lead to loss of consciousness.
Case Description: We present a case of a 65-year-old female who was admitted to a hospital in Phuong Chau, Vietnam in an unconscious state. She had a history of coughing and dyspnea for 1 week. Prior to admission, the patient had dysuria, fever, rigors, hematuria, and increasingly severe flank pain. She had a medical history of hypertension, peptic ulcer disease, and osteoporosis that was treated with losartan. The patient was admitted twice in the previous year for bladder stones. She arrived at the hospital unconscious with a heart rate of 125 beats per minute, blood pressure of 80/50 mmHg, and a mild fever of 100.4 °F/ 37.8°C. She woke up 1 hour after admission and remained lethargic. The patient had mild left costovertebral angle tenderness but denied suprapubic tenderness.
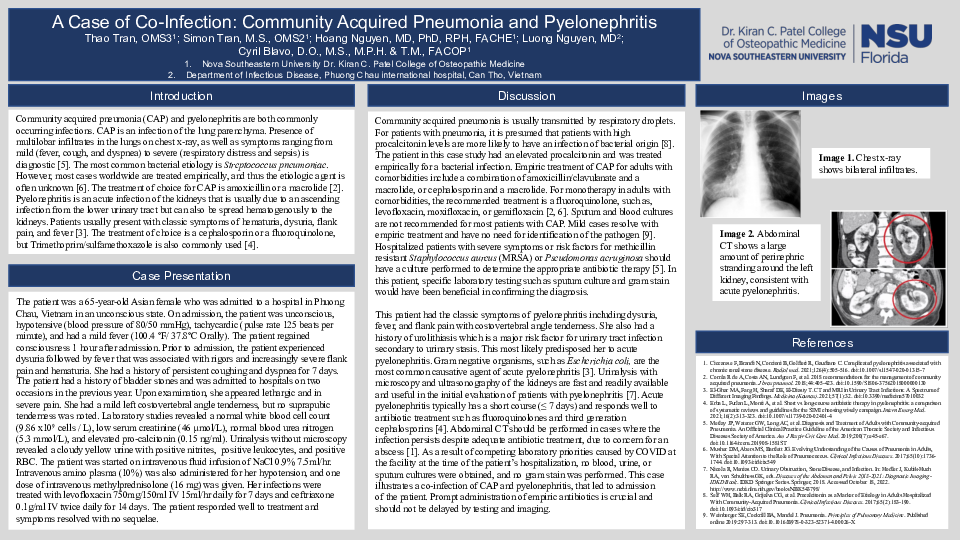
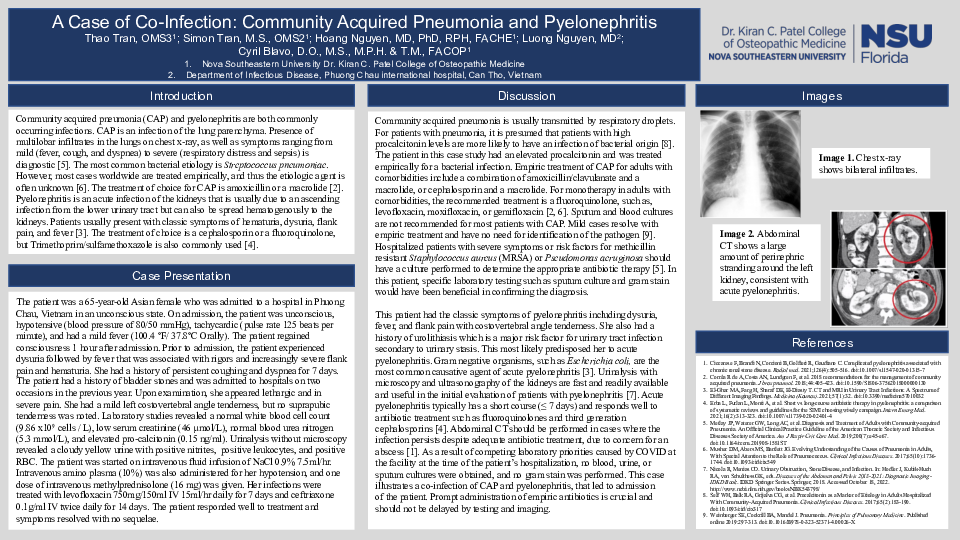
A laboratory assessment included complete blood count, urinalysis, and a basic metabolic panel. Blood work showed normal white blood cell count, a normal level of blood urea nitrogen, low serum creatinine, and elevated pro-calcitonin. Urinalysis exhibited positive nitrites, positive leukocytes, and presence of red blood cells. Her chest x-ray revealed bilateral infiltrates. Single axial and coronal images on abdominal CT showed a large amount of perinephric stranding around the left kidney. The abdominal ultrasound showed a thickened bladder wall with scar tissue from previous bladder stones, but no bladder stones were evident.
The patient was started on intravenous infusion of NaCl 0.9% 7.5ml/hr. Intravenous amino plasma (10%) was also administered for her hypotension, and one dose of intravenous methylprednisolone (16 mg) was given. Her infections were treated with levofloxacin 750mg/150ml IV 15ml/hr daily for 7 days and ceftriaxone 0.1g/ml IV twice daily for 14 days. The patient responded well to treatment and symptoms resolved with no sequelae.
Discussion: This case illustrates a co-infection of CAP and pyelonephritis, that led to admission of the patient. Prompt administration of empiric antibiotics is crucial and should not be delayed by imaging.