Abstract
Background
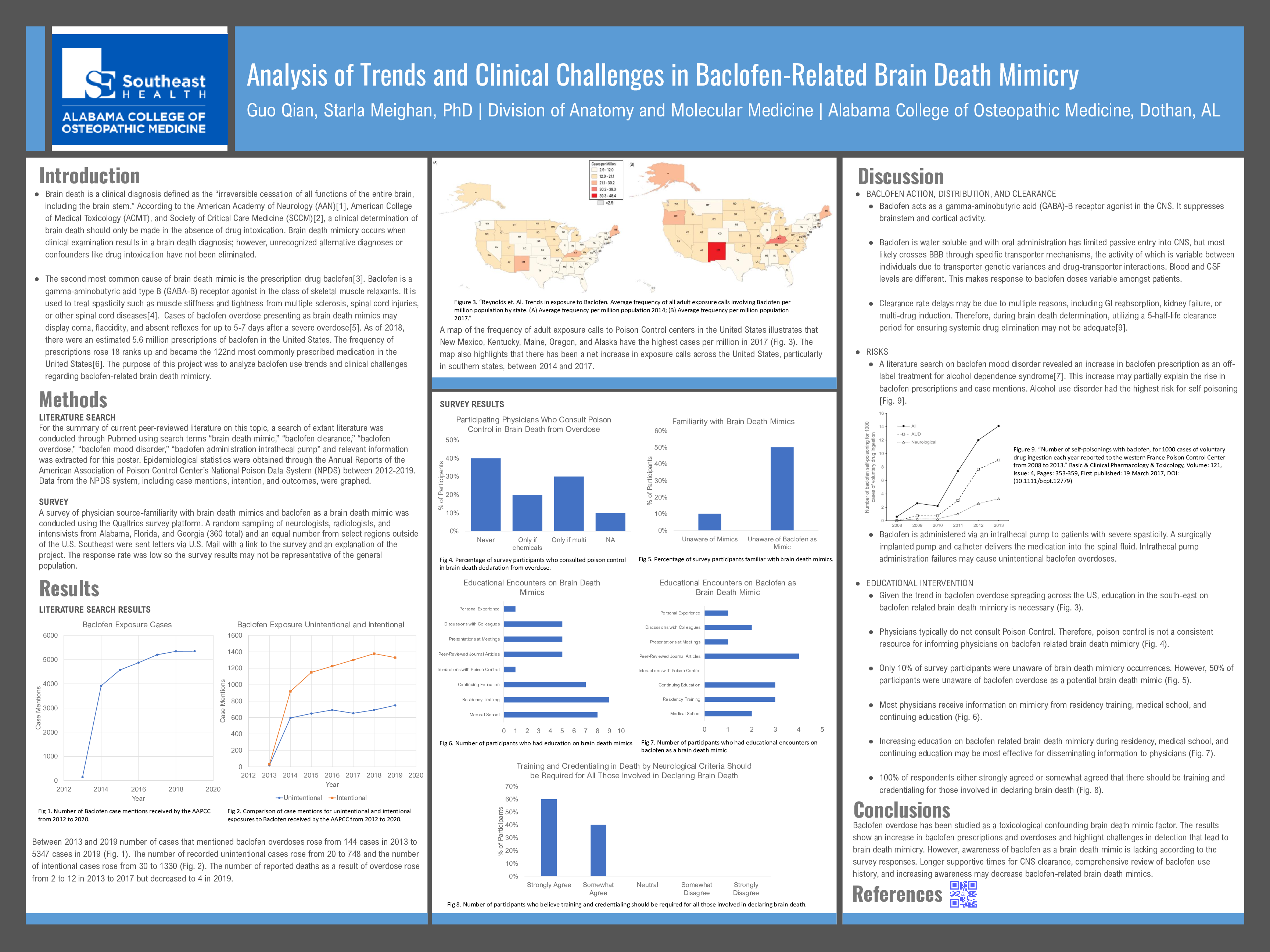
Brain death is a clinical diagnosis made in the absence of drug intoxication that determines irreversible cessation of all functions of the entire brain, including the brainstem. Brain death mimicry occurs when clinical examination results in a brain death diagnosis; however, unrecognized alternative diagnoses or confounders like drug intoxication have not been eliminated. The second most common cause of brain death mimicry is the prescription skeletal muscle relaxant baclofen. The purpose of this project was to analyze baclofen use trends and clinical challenges regarding baclofen-related brain death mimicry.
Study Design
A PubMed literature search and epidemiological statistics through the Annual Reports of the American Association of Poison Control Center’s National Poison Data System (NPDS) between 2012-2019 was conducted. Furthermore, a survey of United States physicians about brain death awareness and training was conducted.
Results
The NPDS reported an increase in baclofen overdose calls to nationwide poison control centers from 144 to 5,347 between 2013 and 2019, respectively. During this period, there was an increase in off-label use of prescribed baclofen to treat alcohol-dependence syndrome. Malfunctioning intrathecal pump or polydrug administration may cause unintentional overdose. Additionally, recent studies indicate five half-lives may be insufficient for estimating complete clearance of baclofen from the central nervous system (CNS). Physician survey data is pending.
Conclusions
The results show an increase in baclofen prescriptions and overdoses and highlight challenges in detection that lead to brain death mimicry. Longer supportive times for CNS clearance, comprehensive review of baclofen use history, and increasing awareness may decrease baclofen-related brain death mimics.