Abstract
Background: In recent years, the expansion of national healthcare coverage has led to an increase in demand for primary care in medically underserved areas and a subsequent shortage of primary care providers to meet these demands. The widespread demand for primary care physicians calls for a better understanding of the factors that influence fourth-year, graduating medical students’ choice to train in residencies located in medically underserved communities. Findings from this research will better inform policies aiming to recruit future fourth-year medical students to train in medically underserved areas.
Objective: To understand the effect of COVID-19 on fourth-year medical students’ decision to train in medically underserved areas, upon graduating medical school.
Methods: A cross-sectional, 49-item online survey studying the factors affecting a fourth-year medical student’s choice for selecting a residency in a medically underserved area was administered to a class of 280 NSU-KPCOM fourth-year medical students. 32 fourth-year students participated in this study, with a response rate of 11.4%.
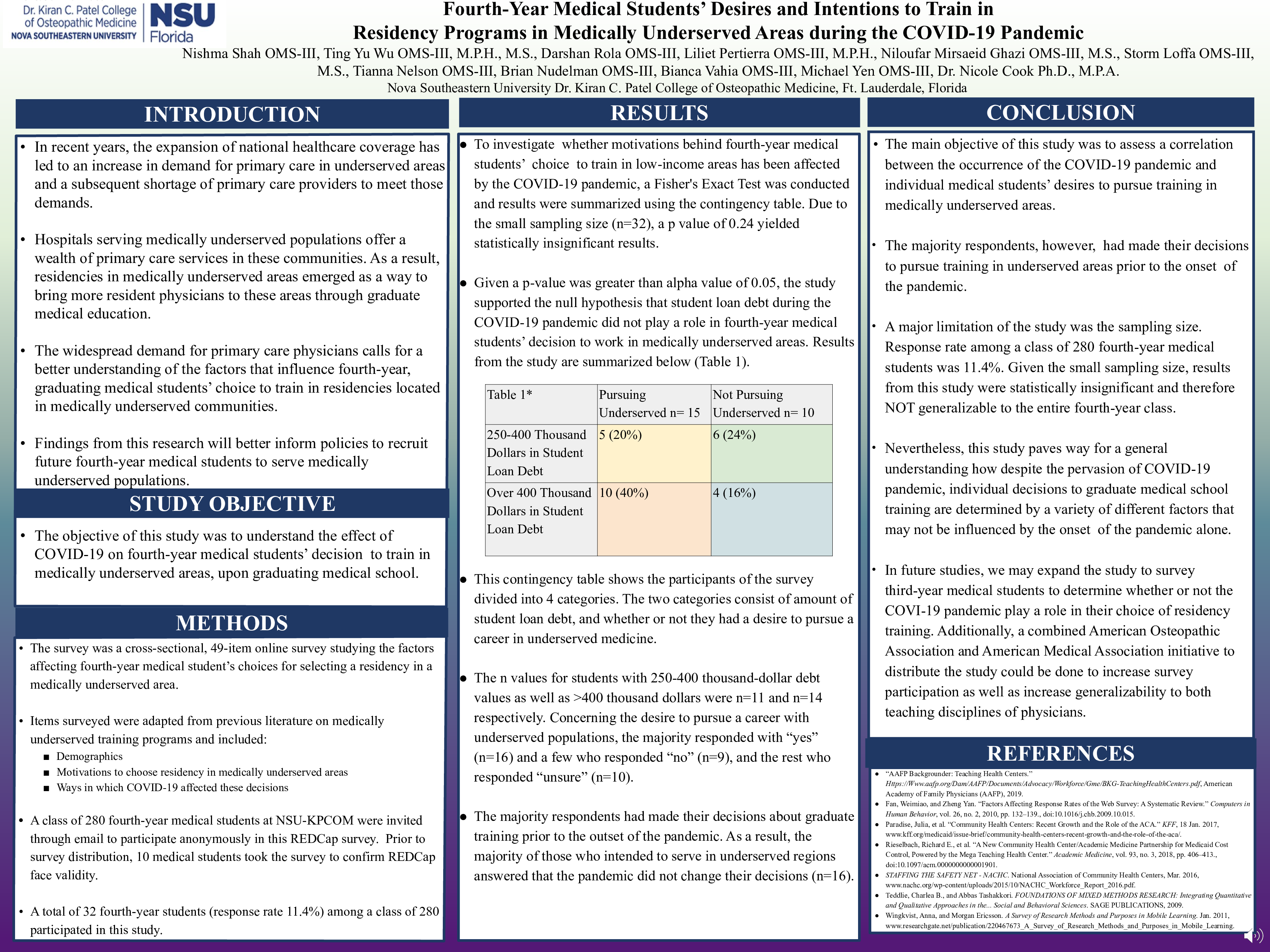
Results: A Fisher's Exact Test was conducted and from the responses obtained from 32 participants, results were summarized using a contingency table. Due to the small sample size, a p value of 0.24 was obtained, providing statistically insignificant results. Since the p-value was less than the alpha value of 0.05, the study supported the null hypothesis that student loan debt during the COVID-19 pandemic did not play a role in fourth-year medical students’ decision to work in medically underserved areas. These results, however, were insignificant.
Conclusion: With a p-value of 0.24, the survey study was unable to determine whether COVID-19 had a statistically significant impact on students’ decision to pursue residency training in medically underserved areas. The main limitation of this study was the sampling size (n=32), which was not large enough to produce statistically significant results. Despite a small sample size, it is still possible that the COVID-19 pandemic had an influence on medical students considering primary care in underserved communities if there was a financial benefit associated with it. With COVID-19 adding complexity to decisions to complete various graduate medical training, it remains critical to understand which factors affect graduating medical students’ pursuit of training in medically underserved areas. As the nationwide shortage of primary care physicians in medically underserved regions continues to be a concerning issue in today’s medical education, it is important to find conclusive answers to the questions we asked in this study on a larger scale of graduating fourth-year medical students. Future studies should expand on this survey approach to capture a wider angle of COVID-19’s impact on fourth-year medical students’ intent to train as resident physicians in medically underserved areas around the nation.