Abstract
Introduction: The right coronary artery (RCA) aberrantly originating from the ascending aorta is extremely rare and makes up 0.04% to 0.15% of reported coronary anatomic variations, with the vessel coursing between the aortic arch and pulmonary trunk being an even rarer subset. Despite normally being an incidental, benign finding, the coronary artery coursing between the great vessels causes compression and predisposes coronary ischemia. Identification and evaluation of these anatomic anomalies are critical to consider for the decision-making process in proper care and to assist in establishing guidelines for the management of patients with similar anatomic variations.
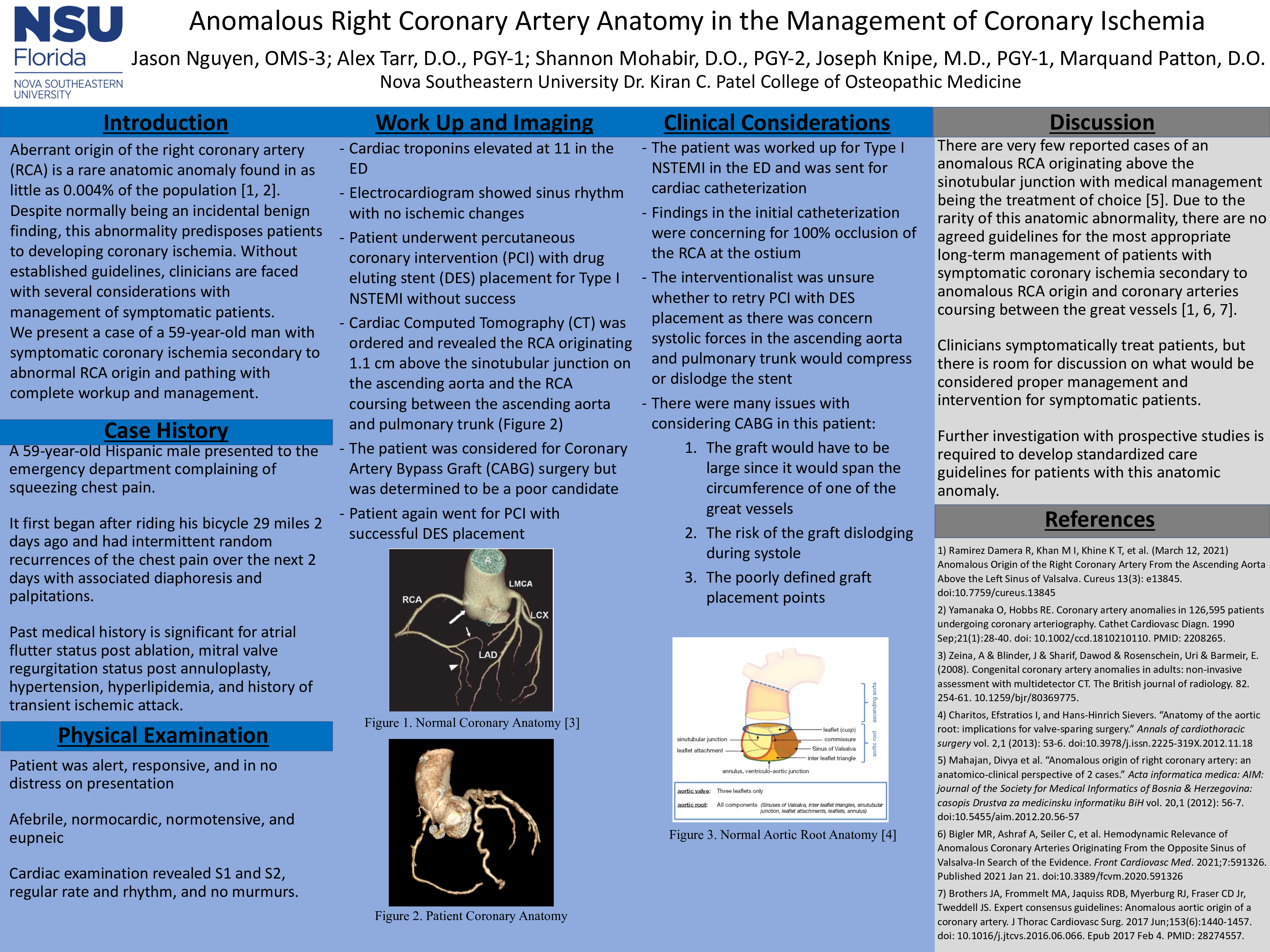
Case Description: We present a case of a 59-year-old Hispanic male with a history significant for atrial flutter status post-ablation, mitral valve regurgitation status post annuloplasty, hypertension, hyperlipidemia, and history of a transient ischemic attack who presented to the emergency department complaining of squeezing chest pain after riding his bicycle 29 miles 2 days ago. Upon returning home, he experienced intermittent random recurrences of the chest pain over the next 2 days and had associated diaphoresis and palpitations. In the emergency department, the patient was alert and responsive, afebrile, normotensive, eupneic, and normocardic. Serum cardiac troponin was elevated at 11, and an electrocardiogram (ECG) showed sinus rhythm with no evidence of ischemic changes. The patient was taken for percutaneous coronary intervention (PCI) for non-ST elevated myocardial infarction (NSTEMI), and findings were concerning for complete RCA occlusion at the ostium. Cardiac Computed Tomography (CT) was ordered to further assess coronary anatomy and revealed the RCA originating 1.1 centimeters above the sinotubular junction, then coursing between the aortic arch and pulmonary trunk before moving laterally. There was concern that if the patient had a drug-eluting stent (DES) placed, the systolic forces from the aortic arch and pulmonary trunk would collapse the DES, rendering treatment ineffective, so coronary artery bypass graft (CABG) surgery was alternatively considered. The cardiac interventionalist reattempted PCI with successful revascularization and DES placement. The patient was discharged with instructions to follow up outpatient regularly with his cardiologist for routine cardiac evaluation.
Discussion: Patients with symptomatic coronary ischemia secondary to abnormal coronary anatomy require close outpatient monitoring with the potential for open surgical intervention if ischemia can be induced. This case highlights the lack of defined guidelines in the management of patients with anomalous coronary anatomy and the changes in approaches to potential treatment options due to pathophysiologic effects of anatomic variation.