Abstract
Introduction: Pancreatitis in the United States has an incidence of 600-700 per 100,000 people. Acute pancreatitis is known to cause acute respiratory alkalosis. Alkalotic derangement can perpetuate lactic acid elevations. We discuss a case of elevated lactate in an alkalotic patient with pancreatitis and liver failure.
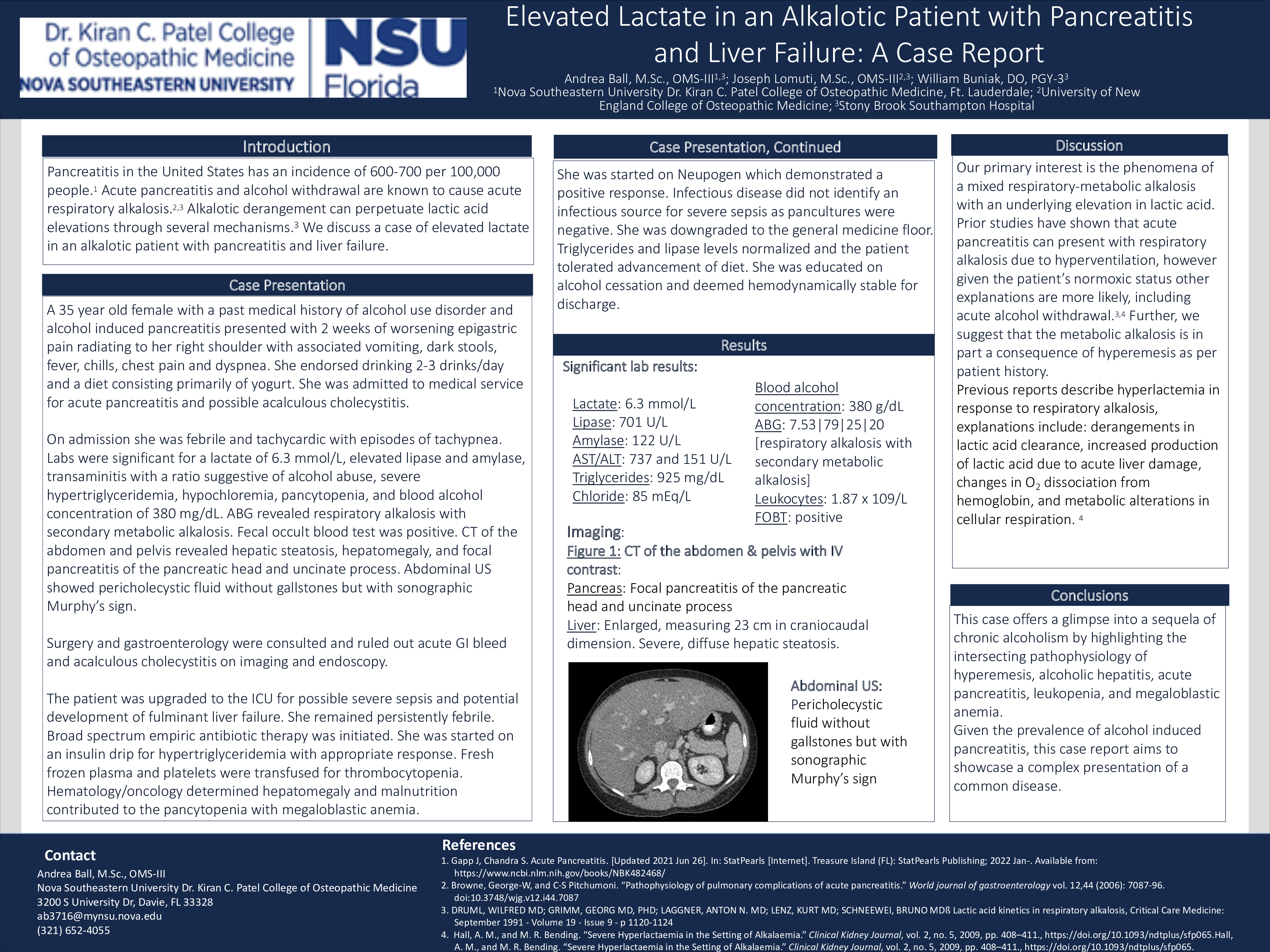
Case Description: A 35 year old female with a past medical history of alcohol use disorder and alcohol induced pancreatitis presented with 2 weeks of worsening epigastric pain radiating to her right shoulder with associated vomiting, dark stools, fever, chills, chest pain and dyspnea. She endorsed drinking 2-3 drinks/day and a diet consisting primarily of yogurt. She was admitted to medical service for acute pancreatitis and possible acalculous cholecystitis. On admission she was febrile at 101.2 F and tachycardic at 108 beats per minute. Labs were significant for a lactate of 6.3 mmol/L, lipase of 701 U/L, amylase of 122 U/L, AST and ALT at 737 U/L and 151 U/L respectively, triglycerides at 925 mg/dL, chloride at 85 mEq/L, and blood alcohol concentration of 380 mg/dL. ABG revealed respiratory alkalosis with secondary metabolic alkalosis with values of 7.53|79|25|20. She was pancytopenic with a white blood cell count of 1.87 x 109/L. Fecal occult blood test was positive. CT of the abdomen and pelvis revealed hepatic steatosis, hepatomegaly, and focal pancreatitis of the pancreatic head and uncinate process. The patient was upgraded to the ICU for possible severe sepsis and potential development of fulminant liver failure. She remained persistently febrile. Broad spectrum empiric antibiotic therapy was initiated. She was started on an insulin drip for hypertriglyceridemia with appropriate response. Surgery was consulted and did not believe the patient required surgical intervention. Gastroenterology ruled out acalculous cholecystitis with a normal HIDA scan and ERCP. No source of bleeding was found on endoscopy. Fresh frozen plasma and platelets were transfused for thrombocytopenia. Hematology/oncology determined hepatomegaly and malnutrition contributed to the pancytopenia with megaloblastic anemia. She was started on Neupogen which demonstrated a positive response. Infectious disease did not identify an infectious source for severe sepsis as pancultures were negative. She was downgraded to the general medicine floor. Triglycerides and lipase levels normalized and the patient tolerated advancement of diet. She was educated on alcohol cessation and deemed hemodynamically stable for discharge.
Discussion: This case offers a glimpse into a sequela of chronic alcoholism by highlighting the intersecting pathophysiology of hyperemesis, alcoholic hepatitis, acute pancreatitis, leukopenia, and megaloblastic anemia. Our primary interest is the phenomena of a mixed respiratory-metabolic alkalosis with an underlying elevation in lactic acid. Prior studies have shown that acute pancreatitis can present with respiratory insufficiency, triggering a compensatory respiratory alkalosis. However, acute pancreatitis with concurrent hypochloremic metabolic alkalosis secondary to hyperemesis is not well documented in the literature. Given the prevalence of alcohol induced pancreatitis, this case report aims to showcase a complex presentation of a common disease.