Abstract
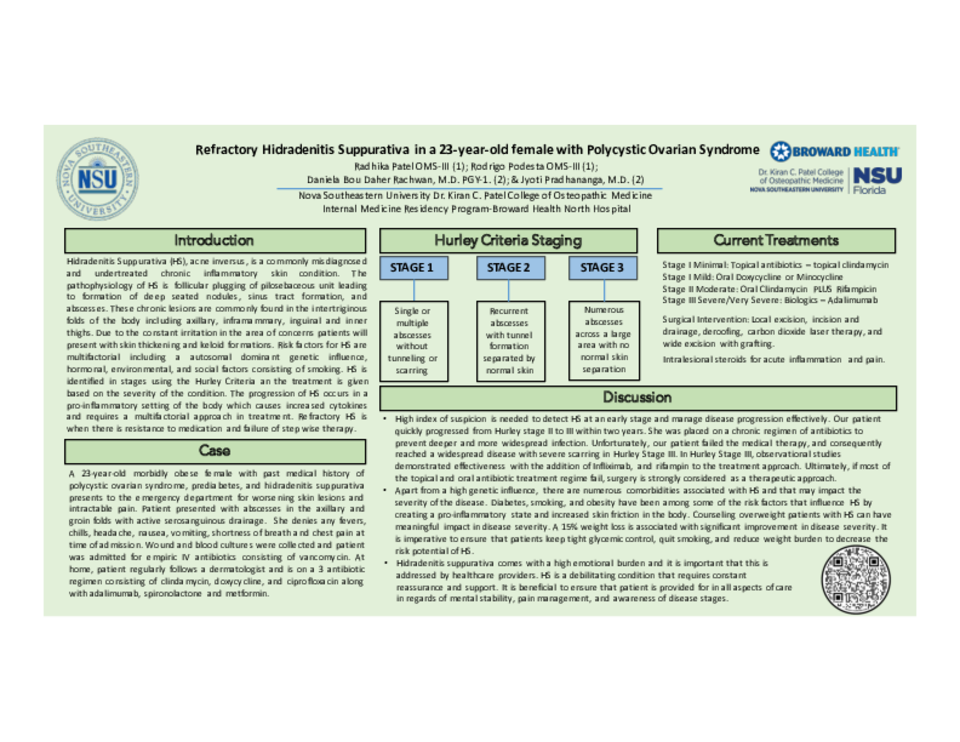
Introduction: Hidradenitis Suppurativa (HS), also known as acne inversus, is a commonly misdiagnosed and underrepresented dermatological condition that affects 1-4% of the population, with the onset of 20-40 years of age, and affecting females at a higher frequency. HS is a chronic inflammatory condition that has genetic influence of 30-45% in an autosomal dominant fashion. The pathophysiology of the condition is follicular plugging of pilosebaceous units leading to deep seated nodules, sinus tract formations, and abscesses. This is a multifactorial condition in which obesity, diet, smoking, and hormonal factors are driving factors in the development and exacerbation of the HS by creating a pro-inflammatory state. HS is clinically diagnosed using the Hurley Staging Criteria (I-III) and treatments are given in a step-wise fashion. It is unclear if these treatments have a high therapeutic value as the condition is still poorly understood. A multifaceted approach is applied ranging from topical and systemic antibiotics, immunomodulating therapies, and surgical interventions. Lifestyle modifications, pain management, and wound care are an integral part of maintaining HS. This is a chronic condition with high emotional and psychosocial burden that requires equal attention and support. Refractory HS is failure of multiple regimen therapy necessitating more aggressive approaches. New methods have shown to minimize the progression of HS that include carbon dioxide laser excision therapy and hyperbaric O2 therapy which promote wound healing, decreased inflammation, and better efficacy of antibiotics.
Case Description: We discuss the case of a 23-year-old African American female patient that presented to us for intractable pain and abscess formation in the axilla and groin area. Past medical history consists of polycystic ovarian syndrome, prediabetes, and morbid obesity. Patient was diagnosed with HS two years ago, currently at Hurley stage 3, on a 3 antibiotic regimen that includes oral clindamycin, ciprofloxacin, and doxycycline, along with a monoclonal antibody, adalimumab with no significant improvement. PCOS and prediabetes are managed with spironolactone and metformin. Family history includes diabetes mellitus and extensive history of HS on her maternal side. She is a non-smoker, and consumes alcohol socially. Upon admission, wound cultures and blood cultures were obtained to further analyze for an infectious process. She was started on empiric IV vancomycin. On skin examination, patient had thickened lesions representing scarring tissue and keloids, associated with active serosanguinous drainage in multiple sites of the axilla and groin. Patient stayed in the hospital for 4 days, received IV antibiotics which were discontinued after blood and wound cultures came back negative. Plastic surgery recommended local excision and skin grafting with hyperbaric O2 therapy. Upon discharge she was restarted on her 3 antibiotic regimen and adalimumab. She was referred to pain management and plastic surgery for outpatient follow up.
Discussion: This case represents the importance of early detection, management of comorbidities to minimize the progression of HS and staying up to date on new therapies to avoid aggressive surgical approaches.