Abstract
Introduction: Acute Promyelocytic Leukemia (APL) is a rare leukemia representing only 5 to 7 percent of all pediatric Acute Myeloblastic Leukemia (AML) cases. There are an estimated 600-800 new cases diagnosed annually in the United States most commonly in adults. APL was once a fatal leukemia due to infections or bleeding that would occur within one month of diagnosis. However, advancements in therapy through the discovery of the PML:RARA translocation mechanism in APL and the introduction of all-trans-retinoic-acid (ATRA), or tretinoin, shifted the dialect of APL as a once fatal leukemia to a highly curable leukemia.
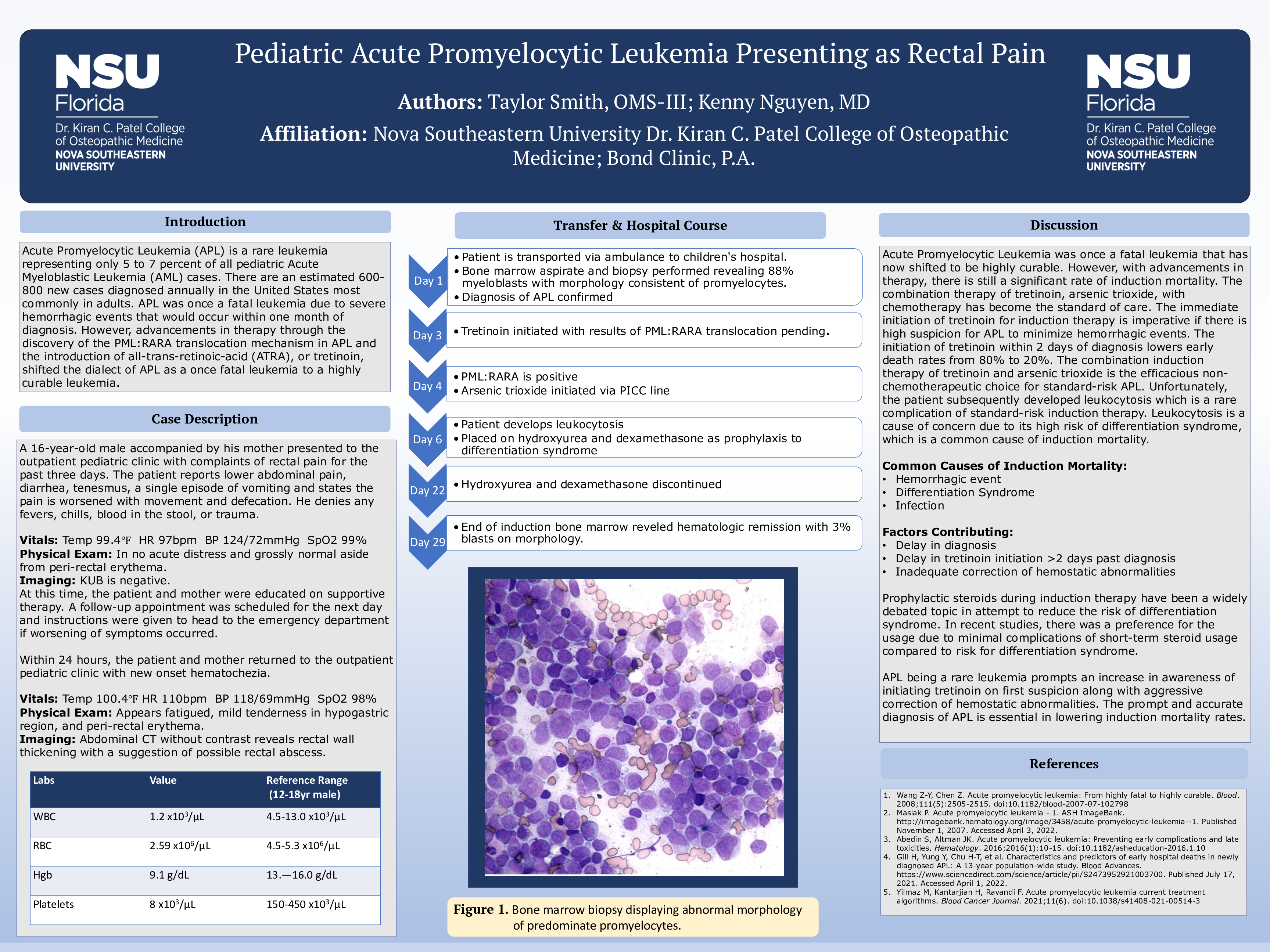
Case Description: A 16-year-old male accompanied by his mother presented to the outpatient pediatric clinic with complaints of rectal pain for the past three days. The patient reports lower abdominal pain, diarrhea, tenesmus, a single episode of vomiting and states the pain is worsened with movement and defecation. He denies any fevers, chills, blood in the stool, or trauma. On presentation, vital signs were found to be stable and physical exam findings were grossly normal aside from peri-rectal erythema. A KUB was ordered with results being negative, at this time the patient and mother were educated on supportive therapy. A follow-up appointment was scheduled for the next day and instructions were given to head to the emergency department if worsening of symptoms occurred. Within the next 24 hours, the patient and mother returned to the outpatient pediatric clinic with new onset hematochezia. The patient now presented as febrile, tachycardic, and displayed mild tenderness in the hypogastric region with continued peri-rectal erythema. At this point, an abdominal CT without contrast was ordered along with a complete blood count, complete metabolic panel, and urinalysis. The CT findings revealed rectal wall thickening with the suggestion of a rectal abscess and the lab work showed pancytopenia with severe thrombocytopenia as a platelet count of 8,000 per microliters of blood. The patient was then transported via ambulance to the nearest children’s hospital. At the children’s hospital, a bone marrow aspirate and biopsy were performed which revealed 88 percent myeloblasts with a morphologic evaluation consistent of promyelocytes. The biopsy confirmed the diagnosis of APL and within two days the patient was started on tretinoin while awaiting results for the PML:RARA translocation. With the translocation present, the initiation of arsenic trioxide was implemented via PICC line. Subsequently, the patient developed leukocytosis and was placed on hydroxyurea and dexamethasone due to the risk for differentiation syndrome. On day 29, end of induction bone marrow aspirate and biopsy was consistent with hematologic remission with 3% blasts on morphology.
Discussion: This case illustrates the prompt and accurate diagnosis of APL is necessary for successful induction therapy.