Abstract
Helicobacter Pylori is a common bacterial infection of the upper gastrointestinal tract affecting up to 50% of the world’s population. Infections are typically chronic and can cause peptic ulcer disease, gastritis, gastric cancer. A common association and possible consequence of H. pylori infection is immune thrombocytopenia. We present a case of unexplained thrombocytopenia in a H. pylori positive patient.
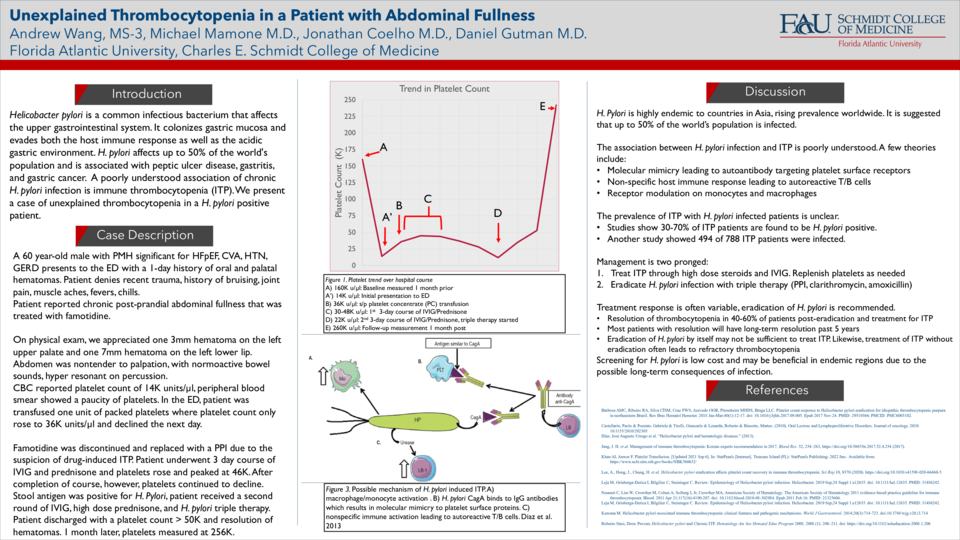
We present a 60-year-old male with a past medical history of heart failure with preserved ejection fraction, recent cerebrovascular accident, who presents with a chief complaint oral hematoma. Additionally, he complained of chronic bloating and abdominal fullness that worsens after eating. Patient was on furosemide, metoprolol, lisinopril for heart failure and famotidine for undiagnosed gastritis/GERD. Patient was hemodynamically stable, in no acute distress, and physical exam was only remarkable for one 7mm hematoma on the left lower lip and an additional 3mm hematoma on the upper left palate. Initial CBC showed a platelet count of 14,000 units/microliter. Peripheral blood smear showed a paucity of platelets. One unit of platelets was transfused in the ED and the subsequent platelet count increased to 34,000 units/microliter. Our initial diagnosis centered around immune-thrombocytopenia due to the marginal improvement in platelet count post transfusion. Per consultation with hematology-oncology, famotidine was discontinued and replaced with a PPI as famotidine is associated with drug-induced ITP. After discontinuing famotidine, however, patient’s platelet count continued to decline. Patient was then started on a 3-day course of IVIG and prednisone. The patient’s platelets began to trend upwards along with resolution of the hematomas, however, upon completion of treatment the patient’s platelets began to decline again. Patient’s bone marrow biopsy was also unremarkable. Upon further literature review, we decided to test for H. pylori stool antigen, which came back positive. Patient was then started on triple therapy for H. pylori (PPI, clarithromycin, and amoxicillin) as well as a second round of IVIG. After completion of his second round of IVIG, the patient was discharged with antibiotics as his platelet count had risen above 50,000 units/microliter. The patient returned two weeks later with a measured platelet count of 256,000 units/microliter.
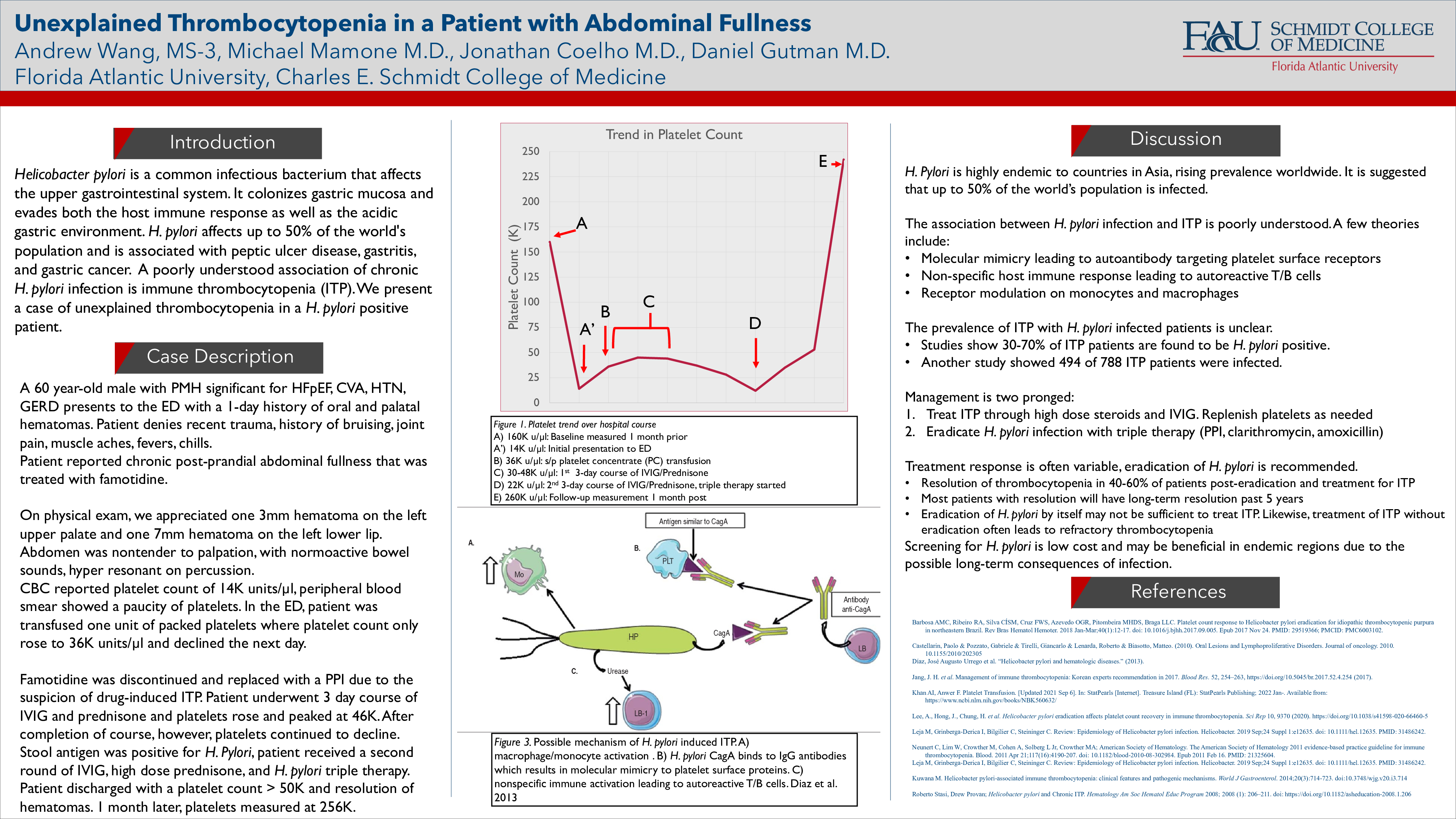
The association between H. pylori and immune thrombocytopenia is unclear and poorly understood. Our current understanding of pathophysiology revolves around molecular mimicry and the formation of autoantibodies generated by H. pylori infection against platelet surface receptors. The prevalence of ITP in H. pylori patients is generally unclear; however, some data has shown that about 30-70% of ITP patients are H. pylori positive. Another study analyzed a population of 788 ITP patients, 494 of whom were infected with H. pylori. Currently, there is conflicting data on whether H. pylori eradication is curative of ITP. This variability in response certainly requires further investigation. Ultimately, this patient presentation bridges two seemingly unrelated symptoms, thrombocytopenia and gastrointestinal complaints. In situations of ITP refractory to treatment, all avenues of possible etiologies must be investigated in order to provide evidence-based patient care.