Abstract
Abstract Title: Elevated White Cell Count in Ascitic Fluid: Not always an infectious cause of ascites.
Author name(s) and title(s): Mizba Baksh, M.B.B.S; Ke Li, MD, Liuyan Jiang, MD; Victoria Alegria, ARNP; Taimur Sher, MD; Vivek Roy, MD; Asher Chanan-Khan, MD; Sikander Ailawadhi, MD; Ricardo D. Parrondo, MD; Muhamad Alhaj Moustafa, MD
Background: Multiple myeloma (MM) is a B-cell neoplasm characterized by clonal proliferation of neoplastic plasma cells in the bone marrow. Extramedullary involvement in the form of malignant myelomatous pleural effusion or ascites is suggestive of a more aggressive disease and is seen in less than 1 % of myeloma cases. Infectious causes of ascites can be differentiated from malignant plasmacytic ascites based on an ascitic fluid cytology and other testing methods such as flow cytometry, immunofluorescence, or electron microscopy.
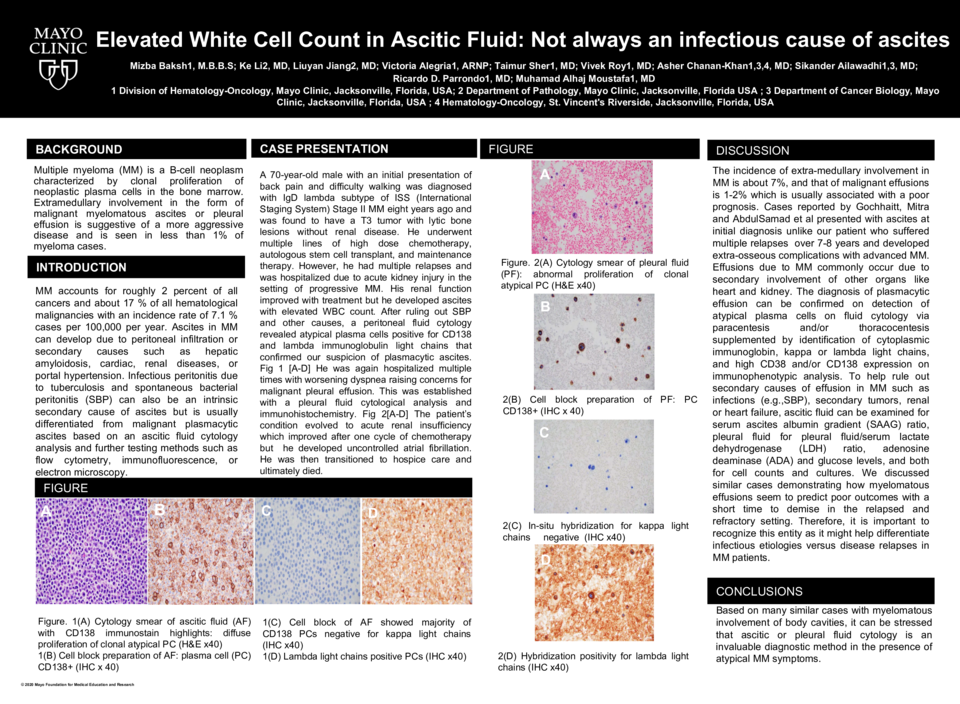
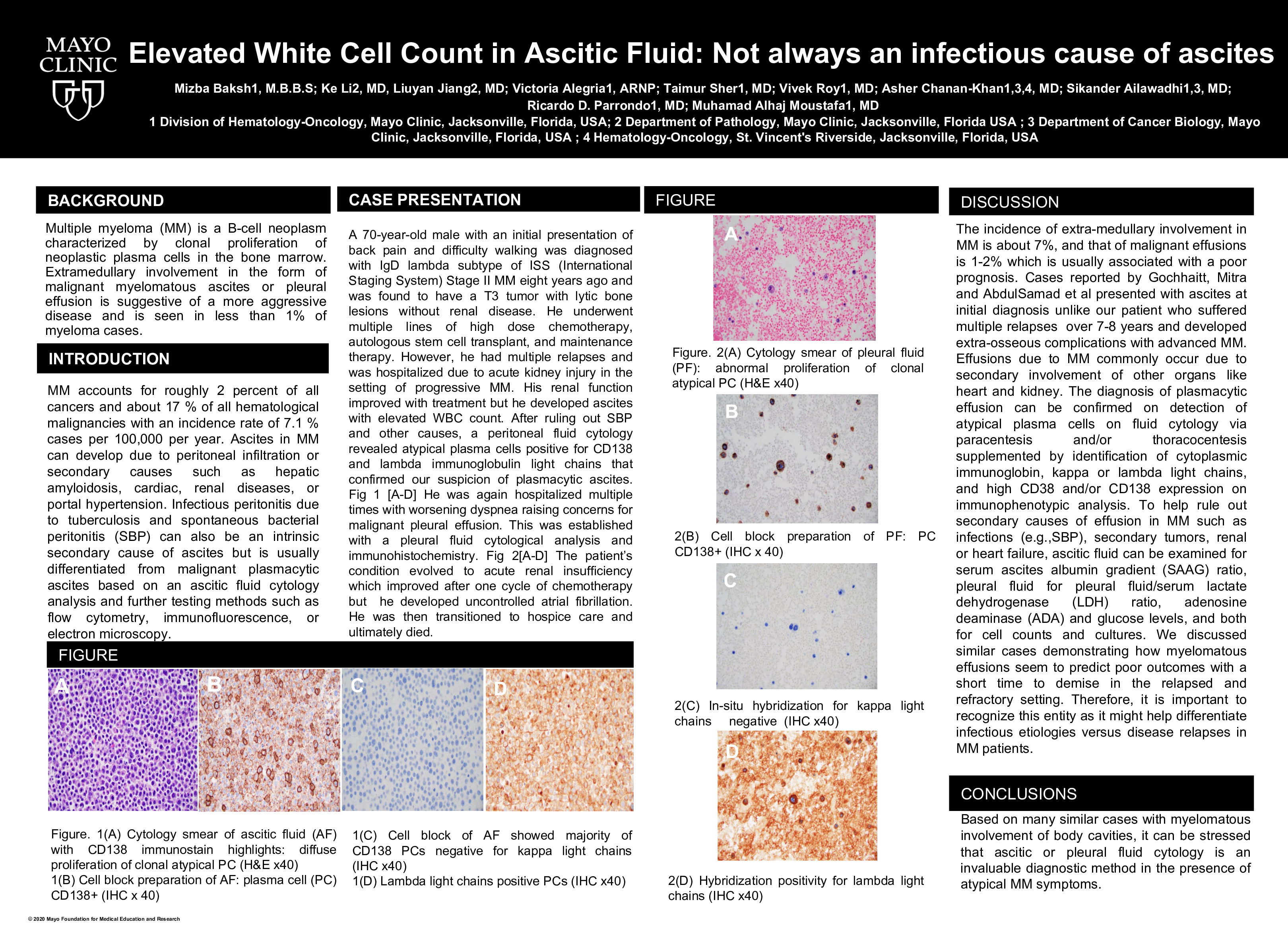
Case presentation: A 70-year-old male with an initial presentation of back pain and difficulty walking was diagnosed with primarily IgD lambda subtype of ISS (International Staging System) Stage II MM eight years ago and was found to have a T3 tumor with lytic bone lesions without renal disease. Despite high dose chemotherapy and autologous stem cell transplant, the patient developed multiple relapses with new lytic lesions and systemic complications and underwent multiple lines of therapy. While still on treatment he was hospitalized with acute kidney injury when he developed ascites with elevated WBC count. After ruling out SBP and other causes, a peritoneal fluid cytology revealed atypical plasma cells positive for CD138 and lambda immunoglobulin light chains that confirmed our suspicion of plasmacytic ascites in the setting of progressive MM. Within one month, his condition rapidly worsened requiring repeated hospitalizations for worsening dyspnea that raised concerns for malignant pleural effusion. The diagnosis was established with a pleural fluid cytology and immunohistochemistry. The patient’s condition evolved into acute renal insufficiency and uncontrolled atrial fibrillation and was transferred to hospice care and ultimately died.
Conclusions: Based on many similar cases with myelomatous involvement of body cavities, it can be stressed that ascitic or pleural fluid cytology is an invaluable diagnostic method in the presence of atypical MM symptoms. It is also helpful in identifying extra-medullary progression in some cases with aggressive disease requiring prompt evaluation and treatment.