Abstract
Purpose: To highlight the significance of prompt recognition and treatment of NMS in susceptible patients suffering from brain injury and make suggestions regarding treatment of Neuroleptic malignant syndrome in these vulnerable patients.
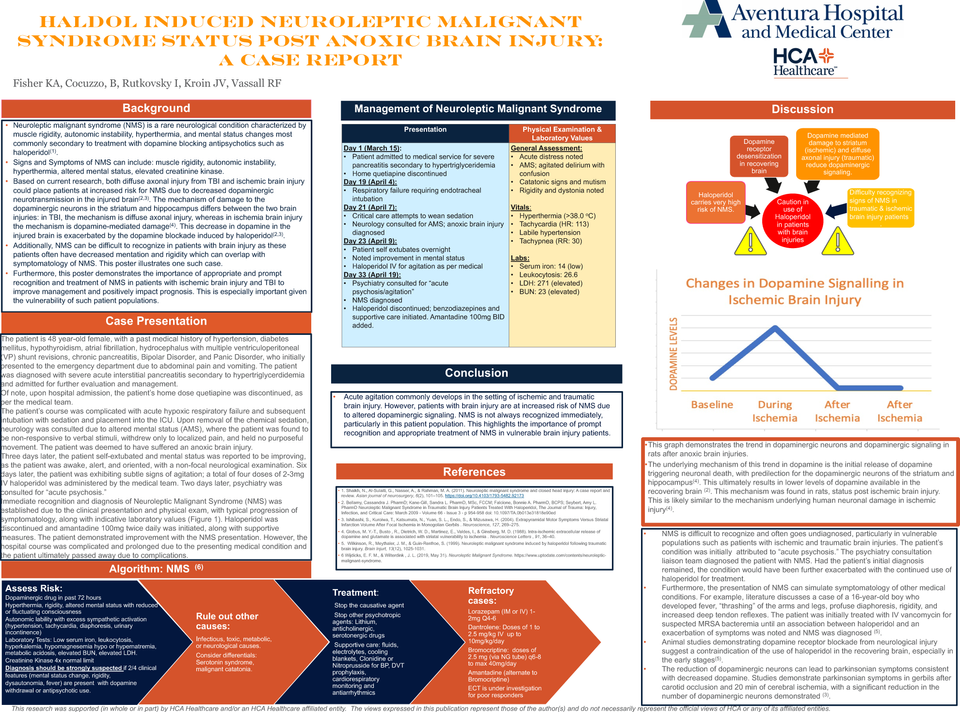
Introduction:Neuroleptic malignant syndrome (NMS), a potentially life threatening, neurological emergency characterized by muscle rigidity, altered mental status (AMS), autonomic instability, and hyperthermia, is most commonly precipitated by high potency, first generation antipsychotics due to central dopamine receptor blockade. Literature indicates a heightened risk of NMS in animals with ischemic or traumatic brain injury due to the resulting death of dopaminergic neurons from injury and the dopamine receptor blockade elicited upon recovery.
Methods: We followed a case which is, to the best of the authors’ knowledge, the first documented case of a critically ill, non-antipsychotic naive patient who suffered an anoxic brain injury with subsequent development of NMS after the initiation of haloperidol for the treatment of acute agitation.
Outcome: The patient was initially admitted for acute pancreatitis and had a prolonged clinical course, she was intubated for respiratory distress and suffered an anoxic brain injury and developed acute agitation. She developed new clinical symptoms after initiation of Haloperidol and was eventually diagnosed with neuroleptic malignant syndrome and Haloperidol was discontinued.
Discussion: Furthermore, NMS can be difficult to diagnose due to variable clinical presentation and lack of absolute diagnostic criteria2, which is further compounded with CNS injury, where neurological abnormalities and AMS may be attributed to the injury, rather than a medication effect, especially in the early period.