Abstract
Introduction: The Ixodes tick may transmit multiple pathogens, Lyme disease being the most common. Patients presenting with the atypical clinical picture of a single pathogen or a lack of improvement with therapy after 48 hours require further testing for the presence of co-infection. We present a case where a patient with atypical symptoms was found to have coinfection with Lyme disease and Babesiosis
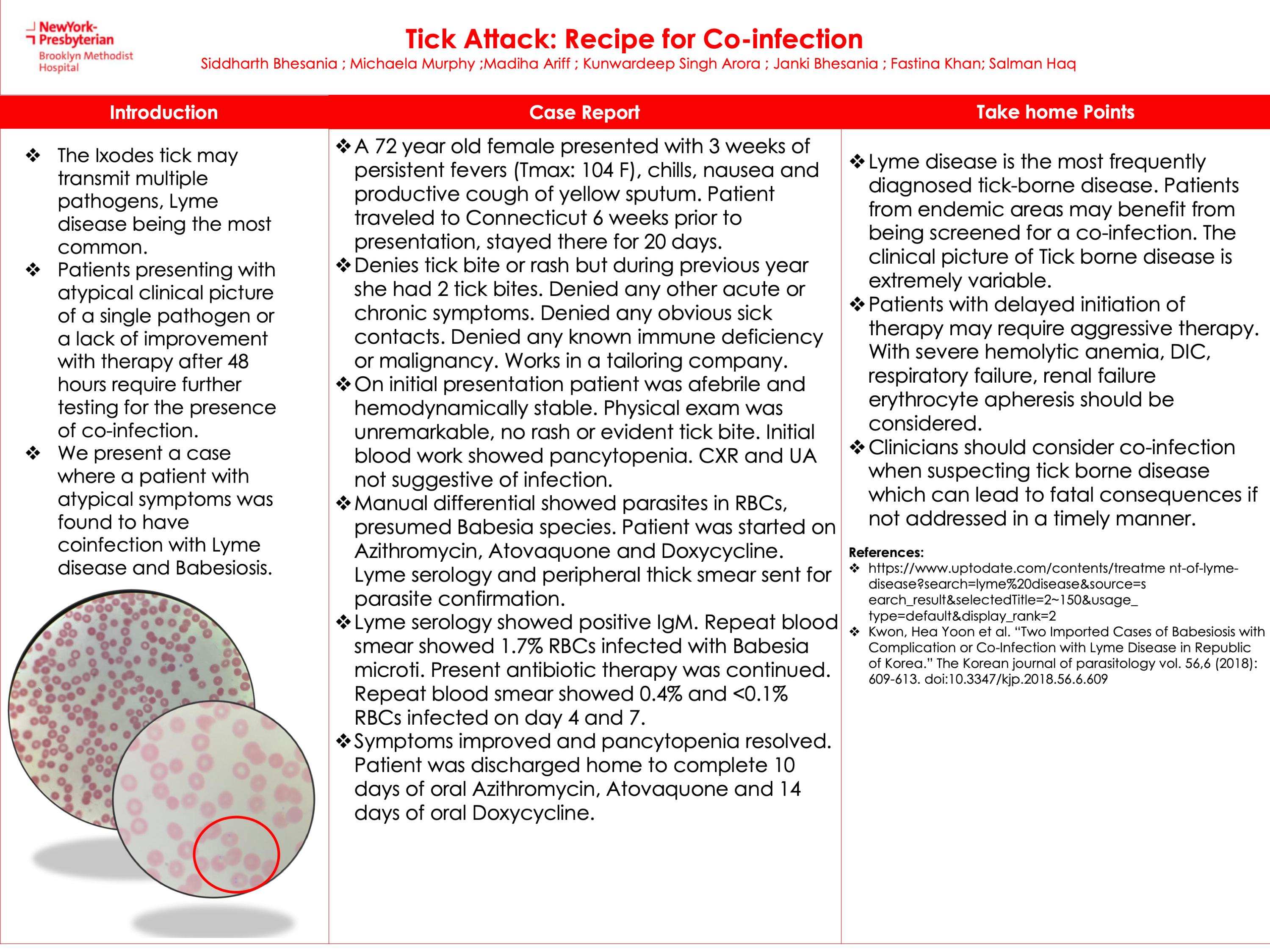
Case presentation: A 72-year-old female presented with 3 weeks of persistent fevers (Tmax: 104 F), chills, nausea, and productive cough of yellow sputum. The patient traveled to Connecticut 6 weeks prior to presentation, stayed there for 20 days. Denies tick bite or rash but during the previous year, she had 2 tick bites. Denied any other acute or chronic symptoms. Denied any obvious sick contacts. Denied any known immune deficiency or malignancy. Works in a tailoring company. On initial presentation, the patient was afebrile and hemodynamically stable. Physical exam was unremarkable, with no rash or evident tick bite. Initial blood work showed pancytopenia. CXR and UA not suggestive of infection. Manual differential showed parasites in RBCs, presumed Babesia species. The patient was started on Azithromycin, Atovaquone, and Doxycycline. Lyme serology and peripheral thick smear were sent for parasite confirmation. Lyme serology showed positive IgM. Repeat blood smear showed 1.7% RBCs infected with Babesia Microti. Present antibiotic therapy was continued. Repeat blood smear showed 0.4% and <0.1% RBCs infected on days 4 and 7 and symptoms improved and pancytopenia resolved. The patient was discharged home to complete 10 days of oral Azithromycin, Atovaquone, and 14 days of oral Doxycycline.
Conclusion: 1. Lyme disease is the most frequently diagnosed tick-borne disease. Patients from endemic areas may benefit from being screened for a co-infection. The clinical picture of Tick-borne disease is extremely variable.
2. Patients with delayed initiation of therapy may require aggressive therapy. With severe hemolytic anemia, DIC, respiratory failure, renal failure erythrocyte apheresis should be considered.
3.Clinicians should consider co-infection when suspecting tick-borne disease which can lead to fatal consequences if not addressed in a timely manner.