Abstract
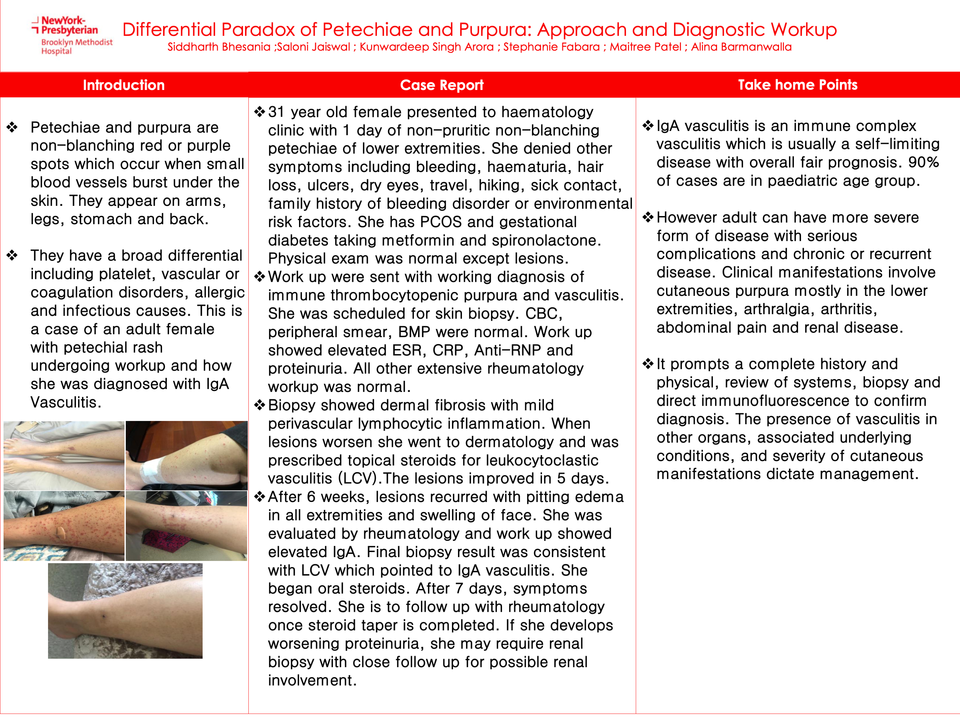
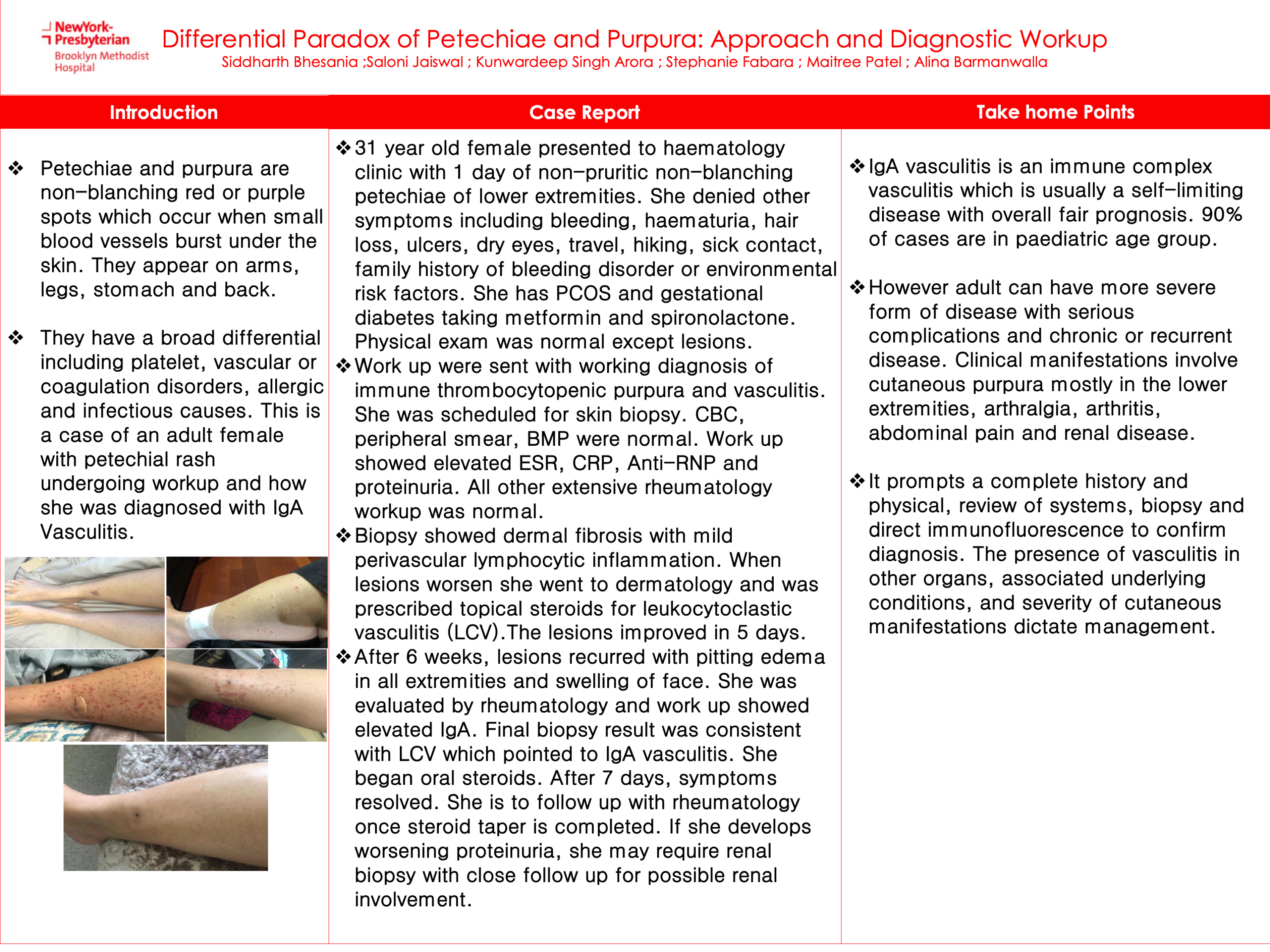
Background:- Petechiae and purpura are non-blanching red or purple spots that occur when small blood vessels burst under the skin. They appear on arms, legs, stomach, and back. They have a broad differential including platelet, vascular or coagulation disorders, allergic and infectious causes. This is a case of an adult female with petechial rash undergoing workup and how she was diagnosed with IgA Vasculitis.
Aim:- To highlight the approach in diagnosing leukocytoclastic vasculitis
Case presentation:- 31-year-old female presented to hematology clinic with 1 day of non-pruritic non-blanching petechiae of lower extremities. She denied other symptoms including bleeding, haematuria, hair loss, ulcers, dry eyes, travel, hiking, sick contact, family history of a bleeding disorder, or environmental risk factors. She has PCOS and gestational diabetes taking metformin and spironolactone. Physical exam was normal except for lesions. Work up were sent with working diagnoses of immune thrombocytopenic purpura and vasculitis. She was scheduled for a skin biopsy. CBC, peripheral smear, BMP were normal. Workup showed elevated ESR, CRP, Anti-RNP, and proteinuria. All other extensive rheumatology workup was normal. Biopsy showed dermal fibrosis with mild perivascular lymphocytic inflammation. When lesions worsen she went to dermatology and was prescribed topical steroids for leukocytoclastic vasculitis (LCV). The lesions improved in 5 days. After 6 weeks, lesions recurred with pitting edema in all extremities and swelling of the face. She was evaluated by rheumatology and workup showed elevated IgA. The final biopsy result was consistent with LCV which pointed to IgA vasculitis. She began oral steroids. After 7 days, symptoms resolved. She is to follow up with rheumatology once the steroid taper is completed. If she develops worsening proteinuria, she may require a renal biopsy with close follow-up for possible renal involvement.
Conclusion:- IgA vasculitis is an immune complex vasculitis which is usually a self-limiting disease with an overall fair prognosis. 90% of cases are in the pediatric age group. However, adults can have a more severe form of the disease with serious complications and chronic or recurrent disease. Clinical manifestations involve cutaneous purpura mostly in the lower extremities, arthralgia, arthritis, abdominal pain, and renal disease. It prompts a complete history and physical, review of systems, biopsy, and direct immunofluorescence to confirm the diagnosis. The presence of vasculitis in other organs, associated underlying conditions, and severity of cutaneous manifestations dictate management.