Abstract
Introduction
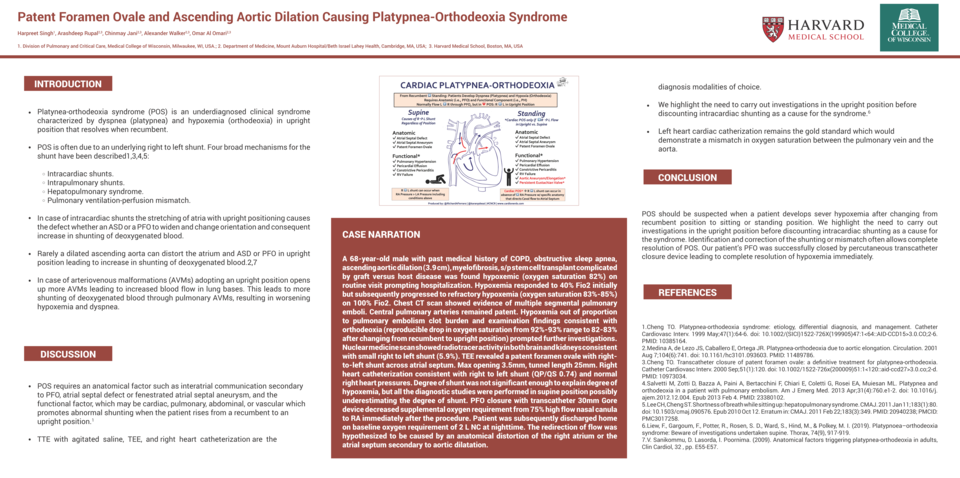
Platynea-orthodeoxia syndrome (POS) is an underdiagnosed clinical syndrome characterized by dyspnea (platypnea) and hypoxemia (orthodeoxia) in an upright position that resolves when recumbent. The pathophysiology was first described in 1949 by Burchell et-al in a patient with an atrial septal defect. Several potential intra-cardiac and pulmonary mechanisms have been described, leading to the increased right-to-left shunting of blood on assuming an upright posture. We report a case of patent foramen ovale (PFO) and dilated ascending aorta presenting as POS.
Case narration
A 68-year-old male with a past medical history of COPD, obstructive sleep apnea, ascending aortic dilation (3.9 cm), myelofibrosis s/p stem cell transplant complicated by graft versus host disease was found to be hypoxemic (oxygen saturation 82%) on a routine visit to his primary care physician, prompting hospitalization. Hypoxemia responded to 40% FiO2 initially but subsequently progressed to refractory hypoxemia (oxygen saturation 83%-85%) on 100% FiO2. Chest CT scan revealed evidence of multiple segmental pulmonary emboli with patent central pulmonary arteries. Hypoxemia out of proportion to pulmonary embolism clot burden and examination findings consistent with orthodeoxia (reproducible drop in oxygen saturation from 92%-93% range to 82-83% after changing from recumbent to an upright position) prompted further investigation. Nuclear medicine scan showed radiotracer activity in both brain and kidneys consistent with a small right-to-left shunt (5.9%). TEE revealed a patent foramen ovale with a right-to-left shunt across the atrial septum, maximum opening 3.5mm, and tunnel length 25mm. A right heart catheterization revealed a right-to-left shunt (QP/QS 0.74) and normal right heart pressures. The degree of the shunt was not significant enough to explain the degree of hypoxemia. However, all the diagnostic studies were performed in a supine position, possibly underestimating the degree of the shunt. PFO closure with transcatheter 30mm Gore device decreased supplemental oxygen requirement from 75% high flow nasal canula to room air immediately after the procedure. The patient was subsequently discharged home on his baseline oxygen requirement of 2 L NC at nighttime. The redirection of flow was hypothesized to be caused by an anatomical distortion of the right atrium or the atrial septum secondary to aortic dilatation.
Discussion
POS is a relatively rare condition. POS requires an anatomical factor such as an interatrial communication secondary to PFO, atrial septal defect or fenestrated atrial septal aneurysm, and a functional factor, which may be cardiac, pulmonary, abdominal, or vascular, that promotes abnormal shunting when the patient rises from a recumbent to an upright position. TTE with agitated saline, TEE, and right heart catheterization may aid in diagnosis. Left heart catheterization remains the gold standard which would demonstrate a mismatch in oxygen saturation between the pulmonary vein and the aorta.
Conclusion
POS should be suspected when a patient develops severe hypoxemia after changing from a recumbent position to a sitting or standing position. Identification and correction of the shunting or mismatch often allow complete resolution of POS. The successful closure of the PFO in our patient via a percutaneous transcatheter closure device immediately led to a complete resolution of his hypoxemia.