Abstract
Context: Glioblastoma is the most common primary malignant neoplasm of the brain affecting adults; with an incidence rate of 3.19 per 100,000 persons in the United States in 2015. Furthermore, the median survival rate is less than 2 years, and the 5-year survival rate is less than 5%. A number of researchers have suggested that socioeconomic and insurance status may be related to shorter glioblastoma survival. However, current scientific information is scant. Understanding and removing barriers to optimal therapy is imperative.
Objectives: To evaluate the association between insurance status (uninsured, Medicaid, or private insurance) and survival in glioblastoma patients after surgery at a population level.
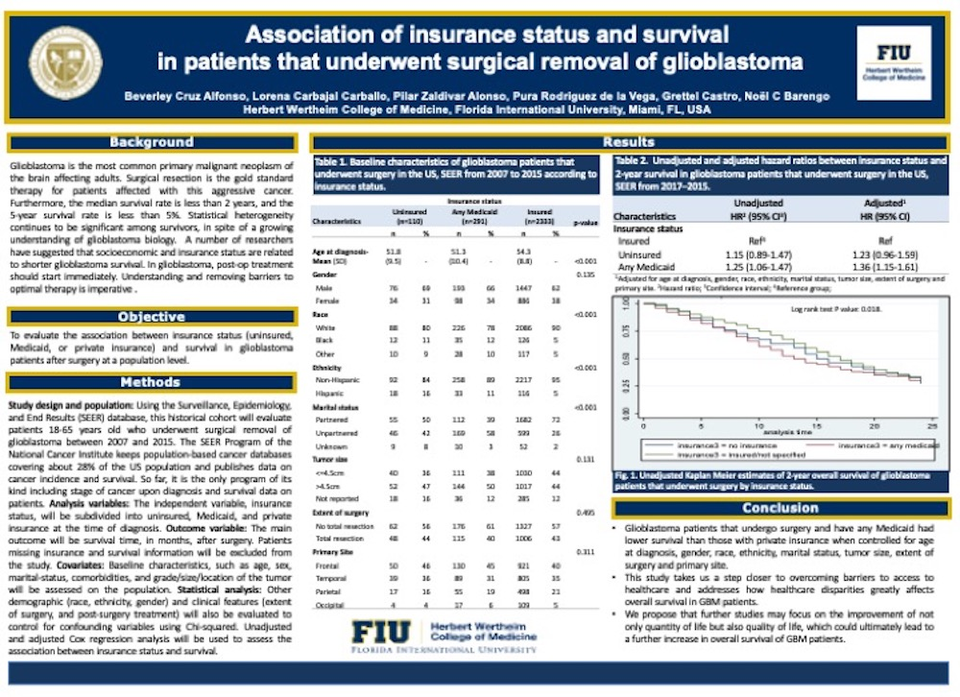
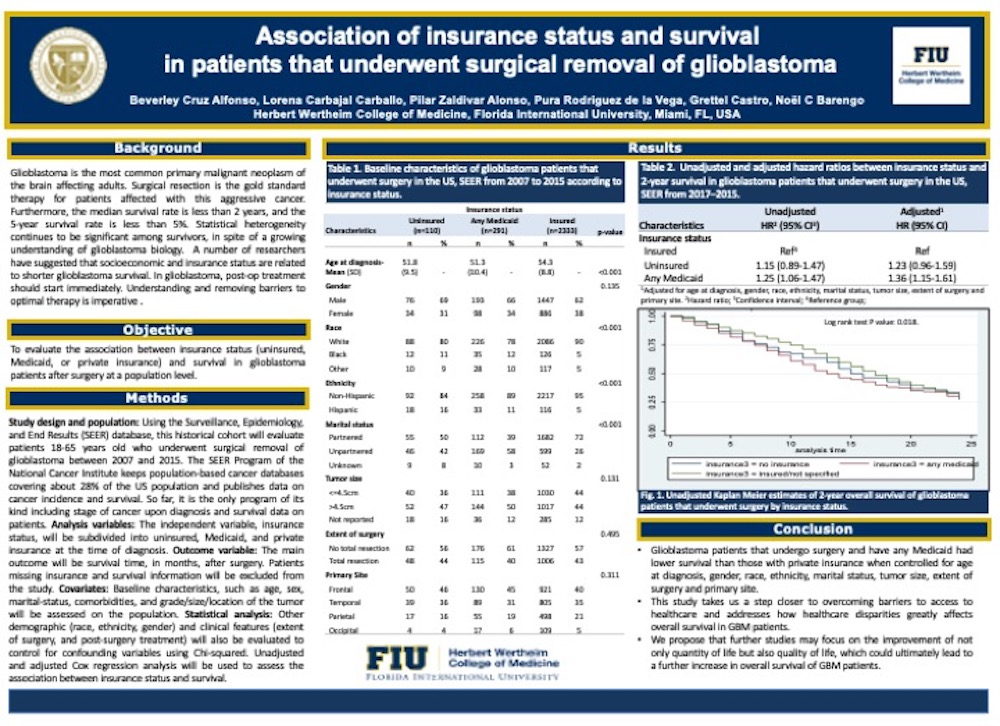
Methods: Using the Surveillance, Epidemiology, and End Results (SEER) database, this historical cohort evaluated patients 18-65 years old who underwent surgical removal of glioblastoma between 2007 and 2015. Patients with missing information on insurance status and survival were excluded from the study. The independent variable, insurance status, was subdivided into uninsured, Medicaid, and private insurance at the time of diagnosis. The main outcome was survival time (measured in months) after surgery. The covariates included were age, sex, marital-status, comorbidities, and grade, size and location of the tumor, race, ethnicity, sex, and extent of surgery, and post-surgery treatment. Unadjusted and adjusted Cox regression analysis were used to assess the association between insurance status and survival. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated.
Results: Out of 2734 glioblastoma patients that underwent surgery, 1616 died in the first two years. The 2-year survival among those with Medicaid was increased by 36% compared with those with a private insurance (HR) 1.36; 95% CI 1.15-1.61). No statistically significant associations were found between being uninsured and survival (HR 1.23; 95% CI 0.96-1.59).
Conclusions: Compared with insured patients, those with any Medicaid have a decreased survival after surgery. Interventions are needed to improve access to healthcare and guarantee insurance coverage in patients with brain malignancies. Future studies may address the outcome disparity between any Medicaid and private insurance, as well as quality of life and its effect on survival.