Abstract
Introduction
Moyamoya disease is a rare occlusive cerebrovascular disease of unknown etiology occurring in a bimodal age. It is a progressive in nature starting from occlusion of the basal ganglia. Moyamoya refers to the “puff of smoke” appearance of the cerebral vasculature on a head CT/MRI arteriography. Despite different pathogenesis, Multiple Sclerosis (MS) and Moyamoya share clinical features such as intermittent neurological symptoms and abnormal neuroimaging.
Case presentation:
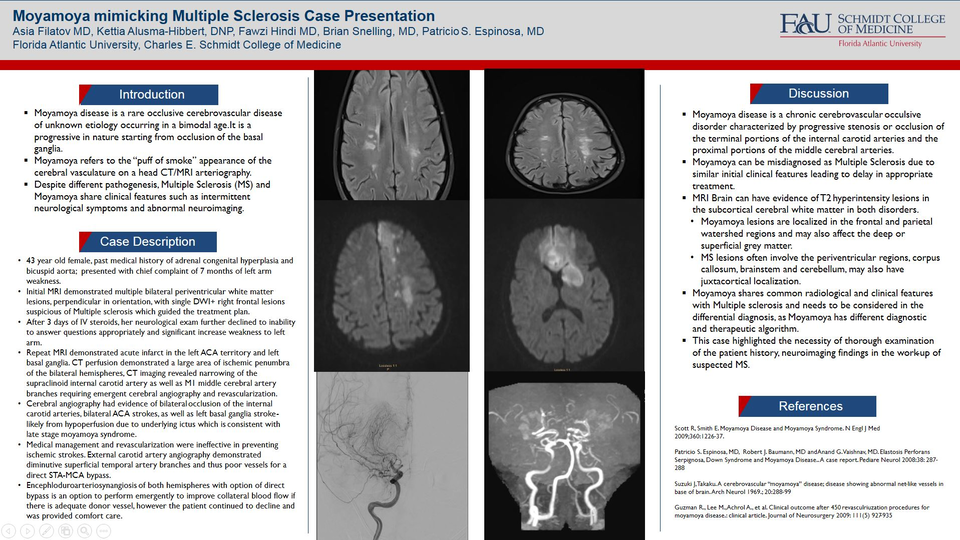
43 year old female, past medical history of adrenal congenital hyperplasia and bicuspid aorta; presented with chief complaint of 7 months of left arm weakness. Initial MRI demonstrated multiple bilateral periventricular white matter lesions, perpendicular in orientation, with single DWI+ right frontal lesions suspicious of Multiple sclerosis which guided the treatment plan.
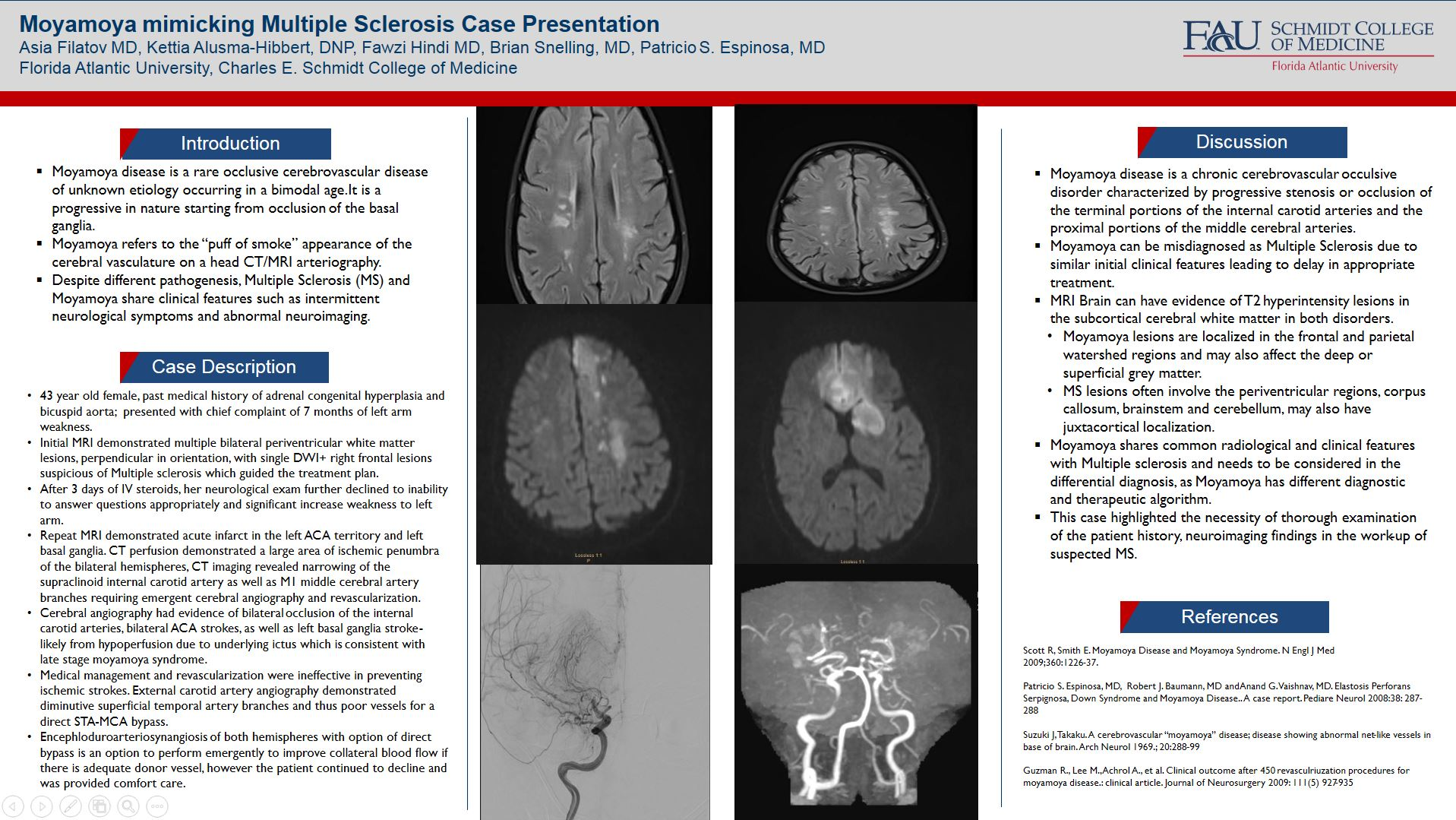
After 3 days of IV steroids, her neurological exam further declined to inability to answer questions appropriately and significant increase weakness to left arm. Repeat MRI demonstrated acute infarct in the left ACA territory and left basal ganglia. CT perfusion demonstrated a large area of ischemic penumbra of the bilateral hemispheres, CT imaging revealed narrowing of the supraclinoid internal carotid artery as well as M1 middle cerebral artery branches requiring emergent cerebral angiography and revascularization. Cerebral angiography had evidence of bilateral occlusion of the internal carotid arteries, bilateral ACA strokes, as well as left basal ganglia stroke - likely from hypoperfusion due to underlying ictus which is consistent with late stage moyamoya syndrome. Medical management and revascularization were ineffective in preventing ischemic strokes. External carotid artery angiography demonstrated diminutive superficial temporal artery branches and thus poor vessels for a direct STA-MCA bypass. Encephloduroarteriosynangiosis of both hemispheres with option of direct bypass is an option to perform emergently to improve collateral blood flow if there is adequate donor vessel, however the patient continued to decline and was provided comfort care.
Discussion:
Moyamoya disease is a chronic cerebrovascular occulsive disorder characterized by progressive stenosis or occlusion of the terminal portions of the internal carotid arteries and the proximal portions of the middle cerebral arteries. Moyamoya can be misdiagnosed as Multiple Sclerosis due to similar initial clinical features leading to delay in appropriate treatment. MRI Brain can have evidence of T2 hyperintensity lesions in the subcortical cerebral white matter in both disorders.Moyamoya lesions are localized in the frontal and parietal watershed regions and may also affect the deep or superficial grey matter. MS lesions often involve the periventricular regions, corpus callosum, brainstem and cerebellum, may also have juxtacortical localization. Moyamoya shares common radiological and clinical features with Multiple sclerosis and needs to be considered in the differential diagnosis, as Moyamoya has different diagnostic and therapeutic algorithm. This case highlighted the necessity of thorough examination of the patient history, neuroimaging findings in the work-up of suspected MS.
References:
Patricio S. Espinosa, MD, Robert J. Baumann, MD and Anand G. Vaishnav, MD. Elastosis Perforans Serpignosa, Down Syndrome and Moyamoya Disease.. A case report. Pediare Neurol 2008:38: 287-288