Abstract
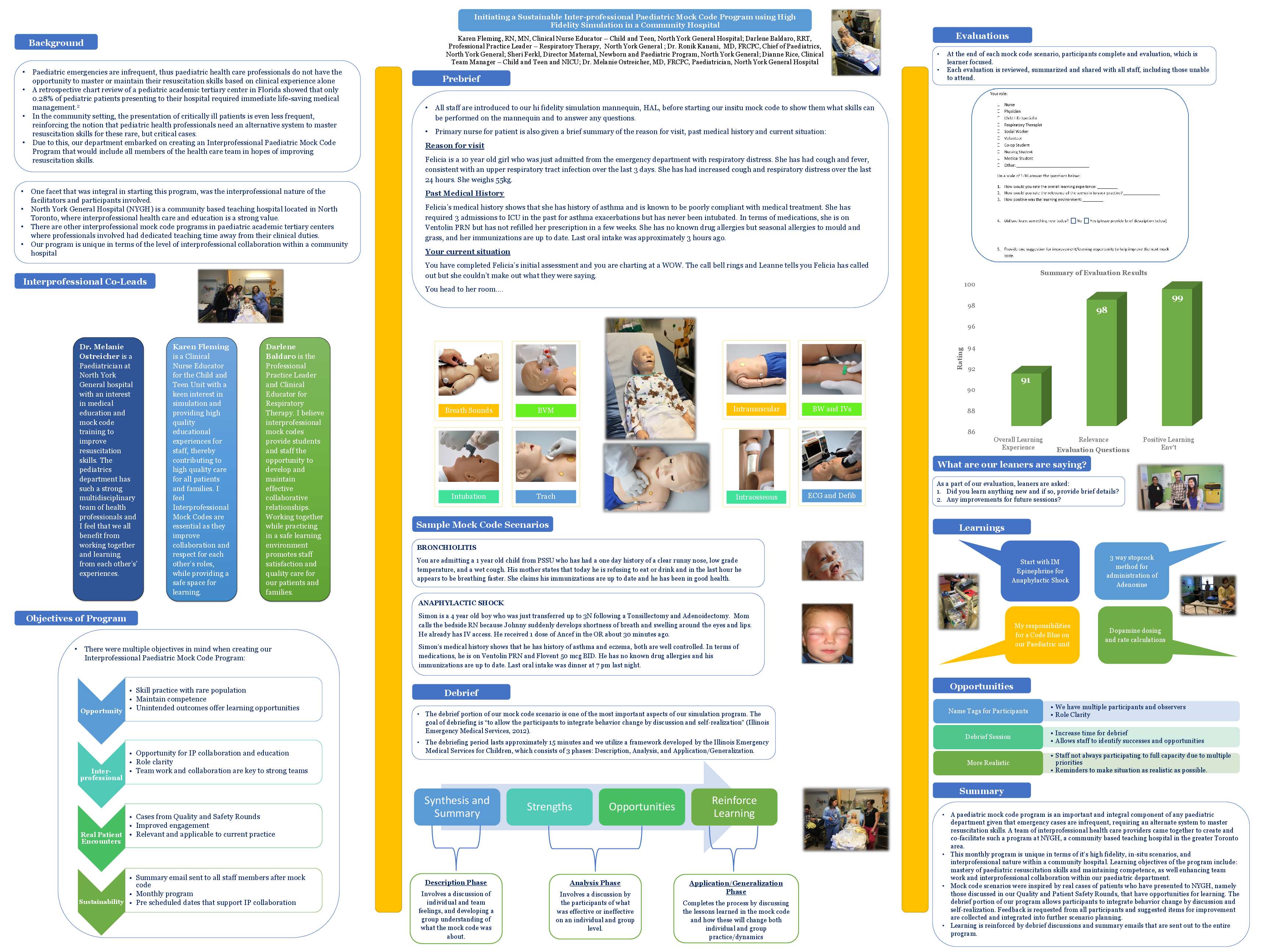
Background/rationale/context: Paediatric emergencies are infrequent, given the nature of illnesses that tend to present in childhood. This reinforces the notion that paediatric health professionals need an alternative system to master resuscitation skills for these rare, but critical cases. Our department embarked on creating an interprofessional paediatric mock code program in the hopes of improving resuscitation skills. In real patient encounters, health professionals who have participated in a mock code program have demonstrated a marked improvement in time to Cardiopulmonary resuscitation (CPR) and defibrillation.4 In creating this program, we are hoping to instill confidence and mastery in health care professionals working on our unit, and improved patient care.
Objective: The objectives included: providing increased interprofessional opportunities for the members of our pediatric unit to practice skills to maintain competency in the care of acutely unwell children; develop effective teamwork skills in the domains of communication, collaboration, and mutual trust and respect; to make a sustainable program that would run on a regular basis.
Description of the innovation: Our monthly paediatric mock code program was initiated in the fall of 2016 by 3 interprofessionals from nursing, respiratory therapy and paediatric medicine. The mock codes are run in situ utilizing a high fidelity mannequin and our scenarios are built around gaps identified from real patient cases presented at our Paediatric Patient Quality and Safety Rounds, where errors and “near misses” are discussed. For each mock code the interprofessional team members are briefly oriented to the simulation mannequin and the primary nurse is given information about the patient’s background. The scenario is followed by a short debriefing period which serves as an opportunity to summarize actions that took place during the code and reflect on the medical management, team communication and procedural skills that occurred.
Impact: Participants anonymously rank their assessment of the overall learning experience, relevance of scenario to their practice and positivity of the learning environment on a rating scale from 1 to 10 and cumulative averages showed rankings of 9.4/10, 9.7/10 and 10/10, respectively. Qualitative feedback from participants identified learning gained in the domains of medical management, procedural skills and practical knowledge. Staff also stated they felt more confident and prepared when dealing with unwell patients in their day-to-day practice.