Abstract
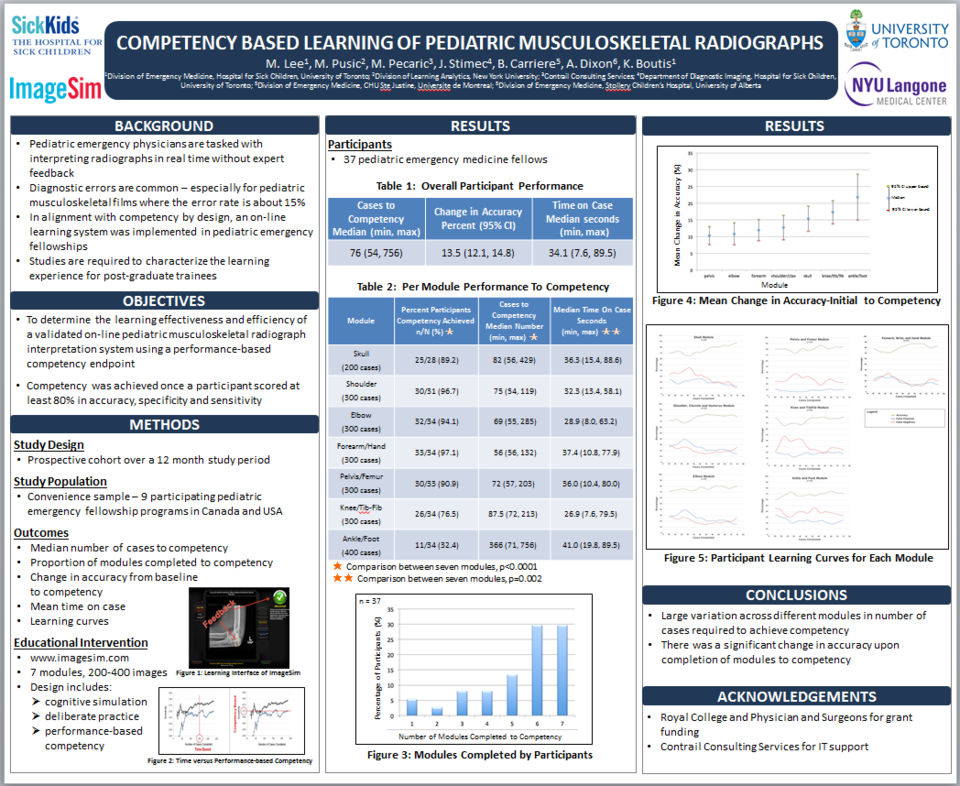
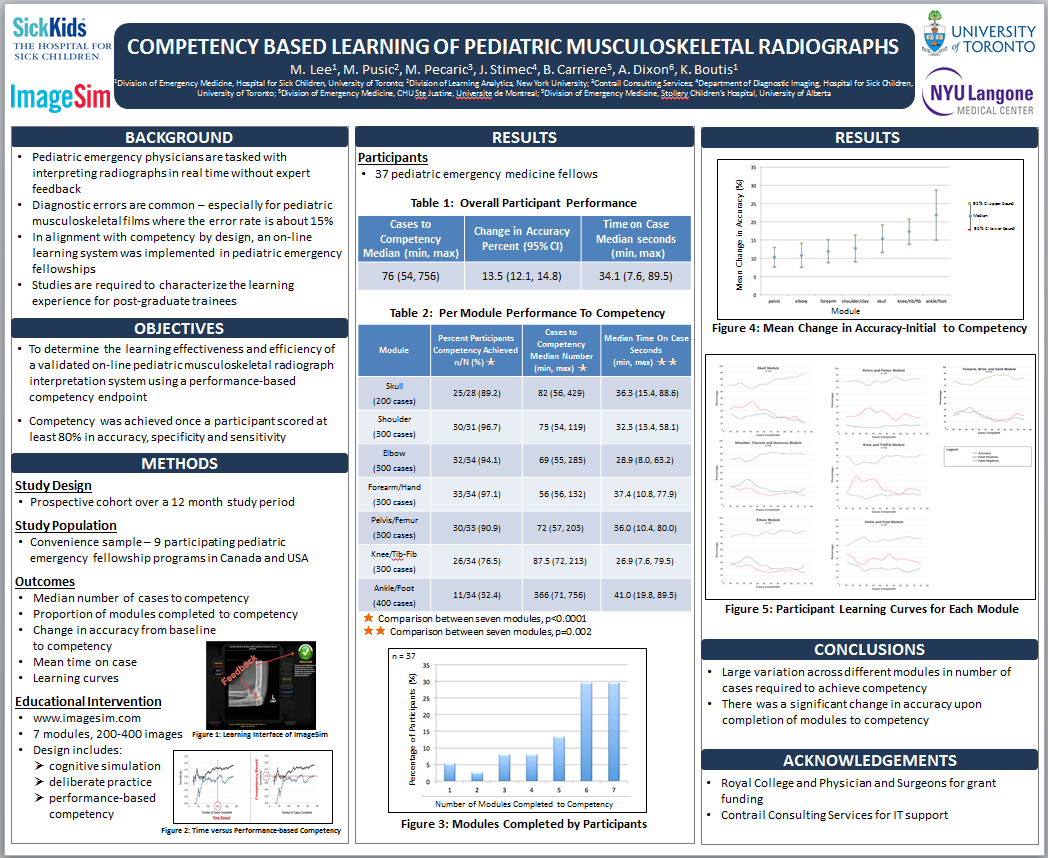
Background: Competency in pediatric musculoskeletal (p-MSK) radiograph interpretation amongst emergency medicine residents is sub-optimal. We have developed ImageSim, a validated education system that uses an “assessment for learning” cognitive simulation platform. The p-MSK course includes seven body regions and cases are practiced using deliberate practice with feedback and continuous assessment (https://imagesim.com/course-information/demo/). Competency is achieved when a participant reaches a pre-set performance benchmark. However, before this can be launched as a residency learning tool standard to help bridge the existing knowledge gap, the education experience for residents should be characterized.
Research Questions: In participating residents, what was the median number of cases required to achieve competency per module and what percent of residents achieved competency in all seven modules? Further, what knowledge gains did the residents experience from baseline to competency and how long did it take them to complete the cases?
Methods: Thirty-five pediatric emergency medicine residents participated for 12 months in this cross-sectional study. Participants did cases until they reached competency, defined as at least 80% accuracy, sensitivity and specificity.
Results: Overall, the median number of cases to competency was 118 (min 56, max 756). The median number of cases to competency per specific module was as follows: skull 67 (56, 129), shoulder 60 (55, 172), elbow 70 (66, 214), forearm-hand 56 (56, 121), pelvis-femur 68 (57, 121), knee-tib/fib 93 (72, 213), and ankle-foot 410 (128, 756), p < 0.001. Eight-five percent of residents completed competency in all seven modules. The mean increase in accuracy from baseline to competency was 13% [95% CI 10, 15)]. The mean time on case 35.8 (SD 0.45) seconds.
Conclusions: Competency was achieved on average in about 120 cases or one hour per module, except for the ankle case-set. Accuracy increased to a competency standard for most participants. Future research could explore the effectiveness of this learning intervention on patient outcomes.