Abstract
Introduction
Delivery of information regarding radiation therapy (RT), using videos, written materials, and one-to-one information sessions have been shown to be effective in reducing anxiety and improving patient satisfaction. Despite the use of a variety of educational delivery methods, breast cancer patients identify gaps in their understanding. The use of virtual simulation in medical education is increasing. There is little research regarding the use of simulation in patient education. The purpose of this study is to use a virtual radiation simulation program to supplement standard educational process for breast cancer patients, to establish impacts on patient knowledge, satisfaction, and anxiety.
Methods
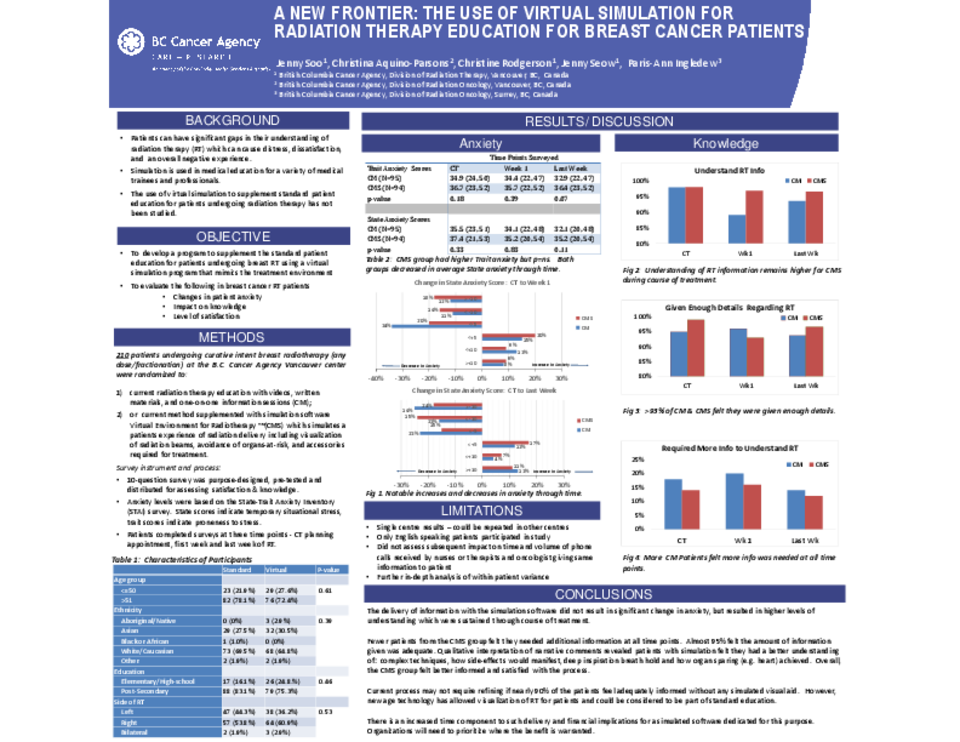
To date, 210 breast cancer patients undergoing curative intent RT at a large academic oncology centre were randomized to one of two educational strategies 1) current RT education with videos, written materials, and one-to-one information sessions (CM) or 2) the current method supplemented with simulated software (CMS). Patients completed a paper based survey at three points in time (CT Simulator appointment, first week of treatment, and last week of treatment). Survey questions were based on needs analysis and designed to assess patient knowledge and satisfaction. Anxiety levels were assessed based on the State-Trait Anxiety Inventory (STAI) questionnaire.
Results
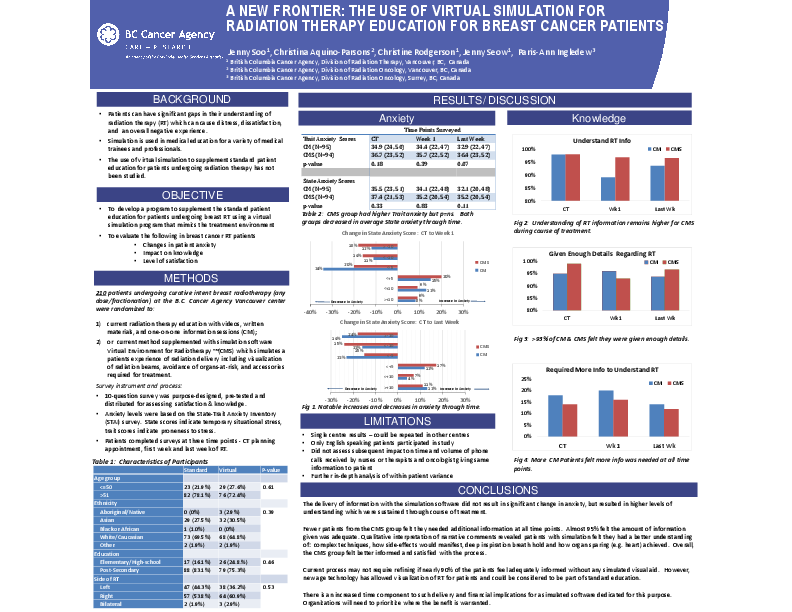
Both groups decreased in average State anxiety scores through time. Mean baseline score at CT for CM was 34.9 and 36.7 for CMS. Almost two-thirds of the all the patients had a decrease in state anxiety by the end of radiation treatment (62% from CM and 54% from CMS). Understanding of RT information remained higher for CMS group during course of treatment. This group also reported they had been given enough details about RT. Patients in the CM group felt more information was needed at all times of their treatment course.
Analysis of narrative comments confirmed the value of the current education method for both arms with patients reflecting that a video, educational pamphlet and one-on-one teaching sessions are important to their learning process. Supplementing with a simulated software provided an opportunity for patients visualize where side effects would manifest, understand special techniques such as deep inspiration breathe hold, and how organ sparing (e.g. heart) is achieved. Overall, the CMS group felt well informed and satisfied with the process.
Conclusion
New technology has allowed visualization of RT for patients. The addition of simulation appears to improve patient knowledge. There is an increased time component to such delivery and financial implications for simulated software dedicated for this purpose. Organizations will need to prioritize where the benefit is warranted. In-depth analysis of data will help to assert if such time considerations are reasonable given the relative gains.