Abstract
Purpose/Objectives(s)
Cancer Care Ontario and the Society of Gynecologic Oncologist guidelines on follow-up for cervical cancer recommend post-treatment surveillance with routine history and physical examination alone in asymptomatic patients. PET is not covered in Ontario; therefore, at our institution MRI is performed 3-6 months following definitive chemoradiation (CRT) as it may detect persistent disease that is surgically salvageable. This study evaluates the utility of follow-up MRI in patients with cervical cancer treated with definitive CRT followed by MR-guided brachytherapy (MRgBT).
Methods/materials
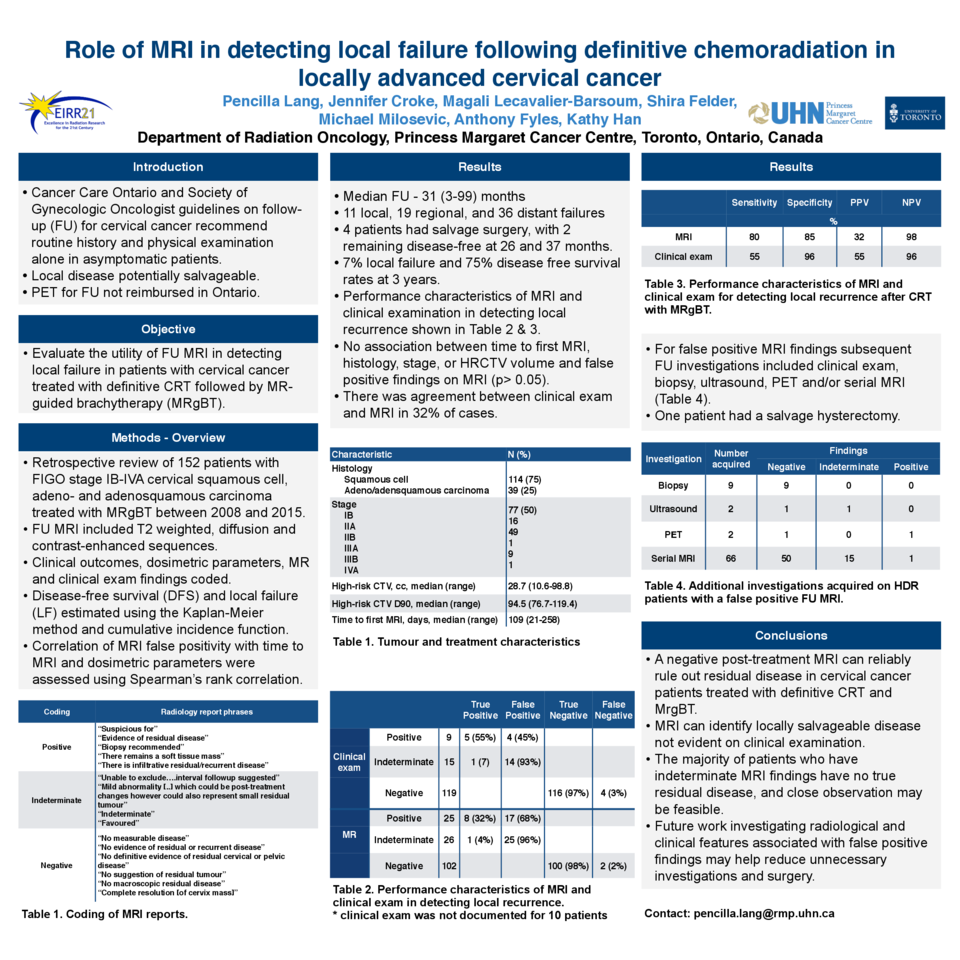
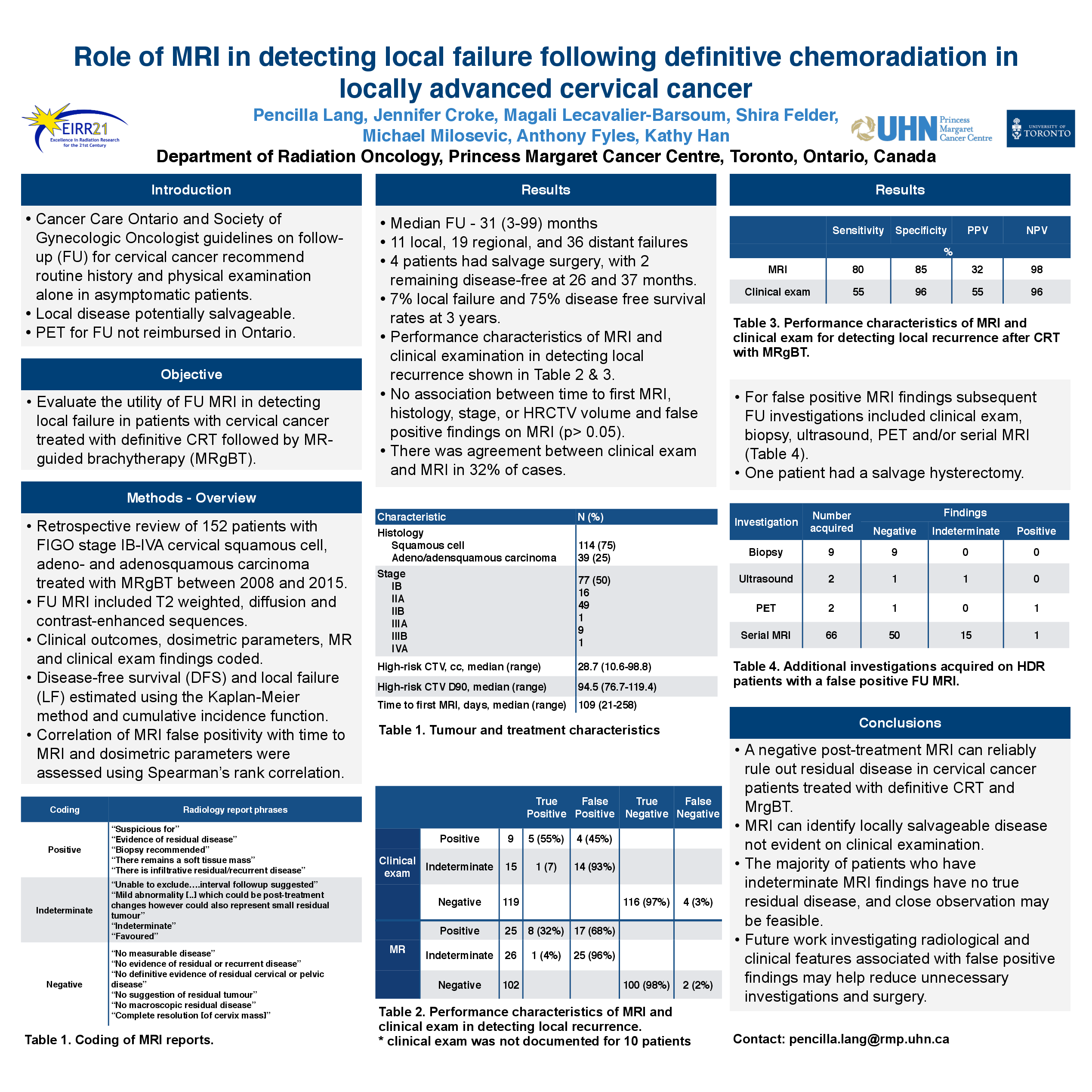
A retrospective chart review was conducted on patients with FIGO stage IB-IVA cervical squamous cell, adeno- and adenosquamous carcinoma who completed definitive CRT with MRgBT between 2008 and 2015. Follow-up MRI included T2 weighted, diffusion and contrast-enhanced sequences. Clinical outcomes, dosimetric parameters, MR and clinical exam findings were recorded and coded. Disease-free survival (DFS) and local failure (LF) were estimated using the Kaplan-Meier method and cumulative incidence function, respectively. Correlation of MRI false positivity with time to MRI and dosimetric parameters were assessed using Spearman’s rank correlation.
Results
Of 153 patients identified, 49% were FIGO stage IB, 43% stage II, 7% stage III and 1% stage IVA. The median high-risk CTV (CTVHR) and D90% were 29cc and 95Gy. With a median follow-up of 31 (3-99) months, there were 11 local, 19 regional and 36 distant failures. The 3-year LF rate was 7% and DFS was 75%. Four patients with isolated LF had salvage surgery. Median time to follow-up MRI was 109 days with 25 reported positive (8 true LF), 26 indeterminate (1 true LF) and 102 negative (2 true LF) for residual disease. Sensitivity/specificity of MRI and clinical exam for LF were 82/86% and 66/86%. MRI detected LF not identified on clinical exam in 2 patients (18% of LF), and correctly excluded LF in 7/14 patients with indeterminate clinical exams. 17/25 patients had false positive MRIs. Subsequent follow-up investigations included clinical exam, biopsy, US, PET and/or serial MRIs, and 2 patients had hysterectomy with no evidence of disease on final pathology. There was no significant correlation between false positive and time to first MRI, CTVHR or D90%.
Conclusions
A negative post-treatment MRI can reliably rule out residual disease in cervical cancer patients treated with definitive CRT and MRgBT. In addition, MR can identify locally salvageable disease not evident on clinical examination. The majority of patients who have indeterminate MRI findings have no true residual disease, and close observation might be feasible. Future work investigating radiological and clinical features associated with false positive findings may help reduce unnecessary investigations and surgery.