Abstract
Introduction
Brain metastases (BM) may cause persistent or episodic neurocognitive impairments which impact a patient’s ability to drive safely. The national standard for licensure requires sufficient motor, sensory and cognitive function and a seizure-free period of at least six months. Assessment of whether a patient meets these criteria often relies on a physician’s judgement. We reviewed documented recommendations regarding driving in a population receiving whole brain radiotherapy (WBRT).
Methods
Demographic, symptom, disease and treatment-related data were abstracted for consecutive adult patients receiving palliative WBRT for BM at our institution (01-12/2015). Prophylactic cranial irradiation, stereotactic and partial brain RT were excluded. Karnosfky Performance Status (KPS) was available in 84.9%. RTOG Neurologic Function Classification (RNFC) was retrospectively assigned. Descriptive statistics were calculated, and a logistic regression model used to identify factors predictive of documentation of discussion of driving restrictions.
Results
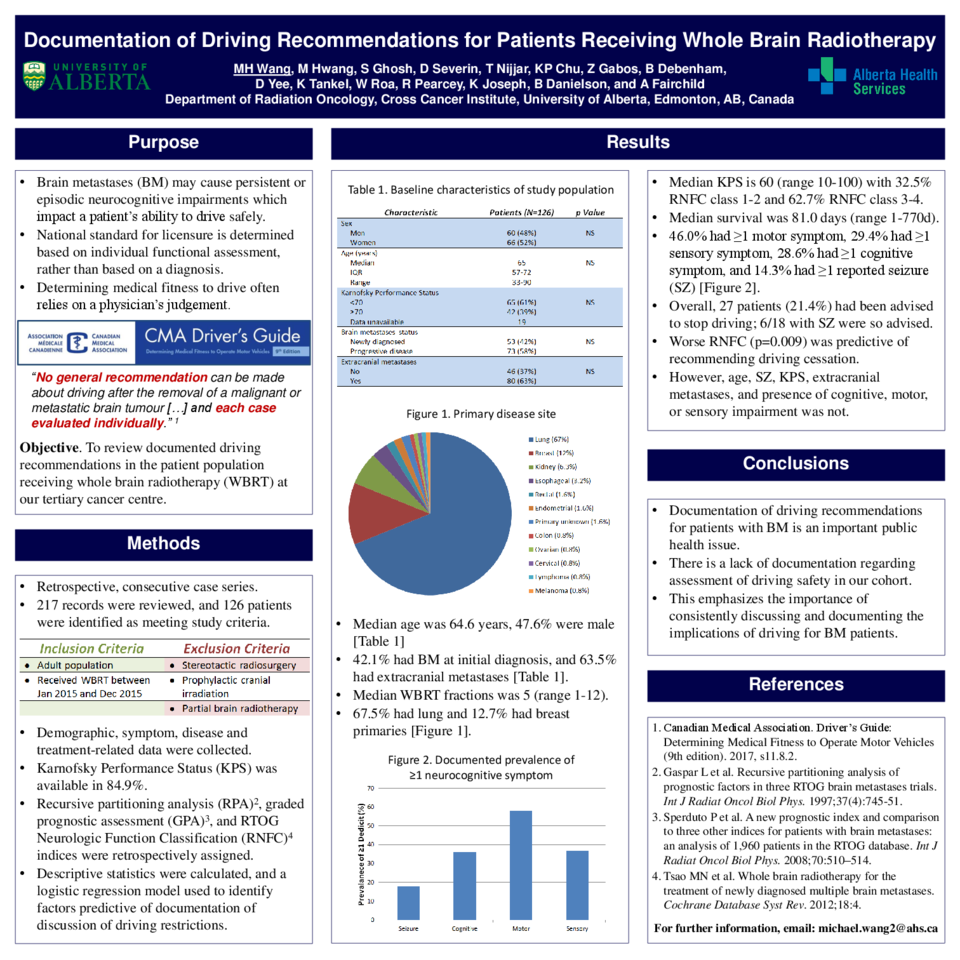
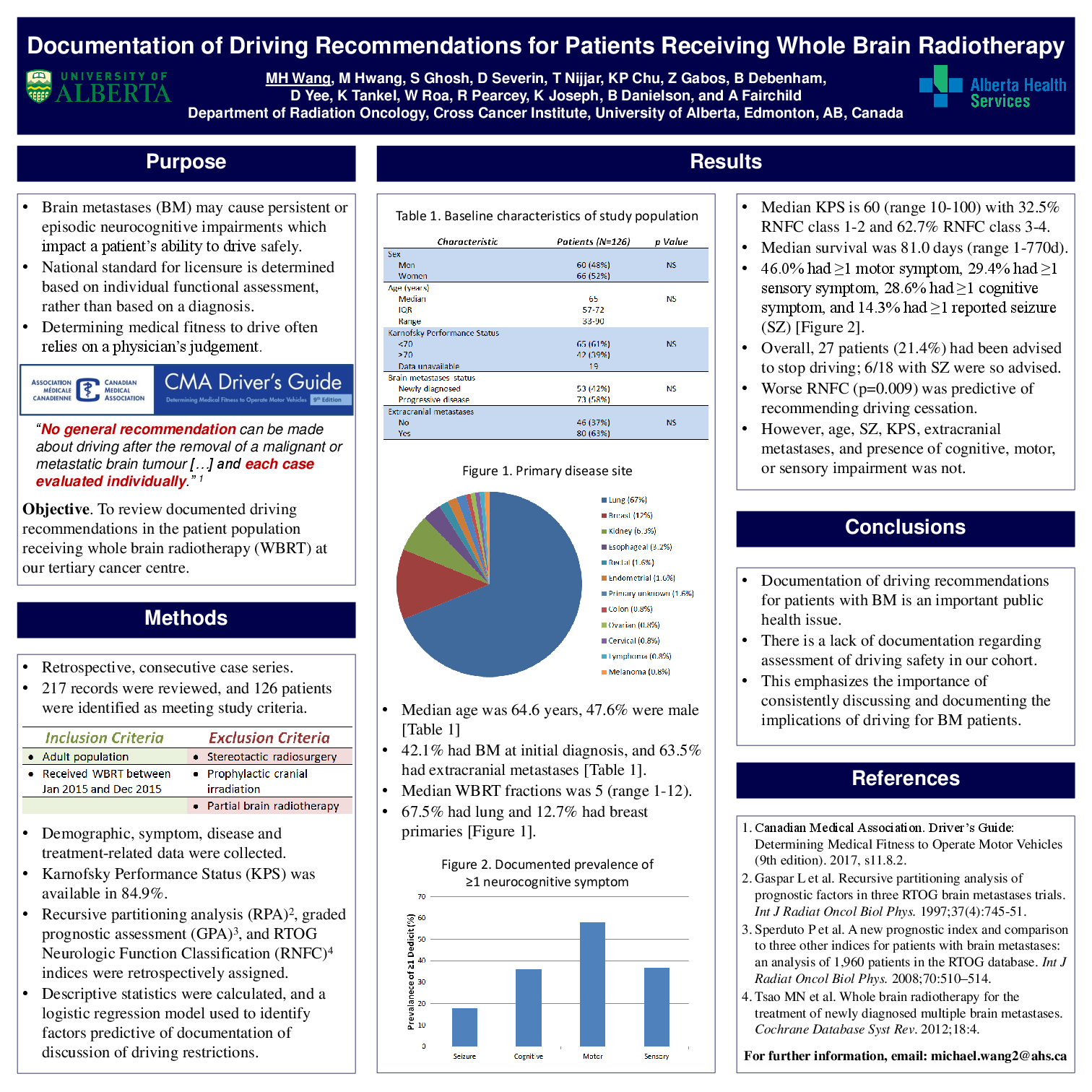
For the 126 eligible patients, median age was 64.6 years, 47.6% were male, 42.1% had BM at initial diagnosis, 8.7% had previous treatment for BM, and 63.5% had extracranial metastases. 67.5% had lung and 12.7% had breast cancer. Median KPS was 60 (range 10-100) with 32.5% RNFC class 1-2 and 62.7% RNFC class 3-4. 46.0% had >1 motor symptom, 29.4% had >1 sensory symptom, 28.6% had >1 cognitive symptom, and 14.3% had >1 reported seizure (SZ). Median WBRT fractions delivered was 5 (range 1-12). Median survival was 81.0 days (range 1-770d). Overall, 27 patients (21.4%) had been advised to stop driving; 6/18 with SZ were so advised. Worse RNFC (p=0.009) was predictive of recommending driving cessation. However, age, SZ, KPS, extracranial metastases, and presence of cognitive, motor, or sensory impairment was not.
Conclusions
Although it is an important public health issue, there is a lack of documentation regarding assessment of driving safety in our cohort of patients receiving WBRT for BM. This finding emphasizes the importance of consistently discussing and documenting the implications of driving for BM patients.