Abstract
Purpose
The use of 3D printer technology to create bolus for radiotherapy (RT) is greatly increasing. At our center, we use an optical scanner to obtain patient surface anatomy images which are used to 3D print a rigid bolus for patients undergoing RT for sarcoma or skin cancer. This bolus is superior to conventional bolus as it produces a more accurate fit with less air gaps, especially in complex treatment areas. At our institution and many others 3D printed bolus is becoming more common and so we set out to analyze time effectiveness and explore staff and patient perception of utilizing 3D printer technology.
Methods
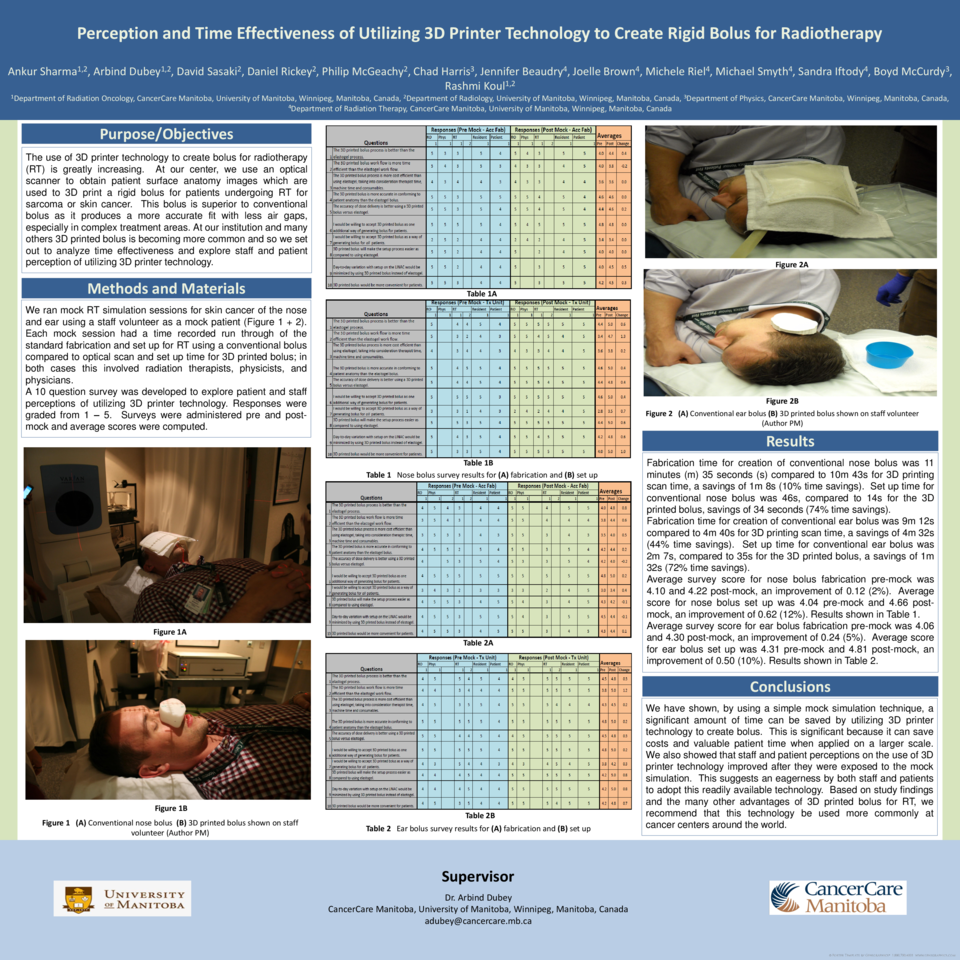
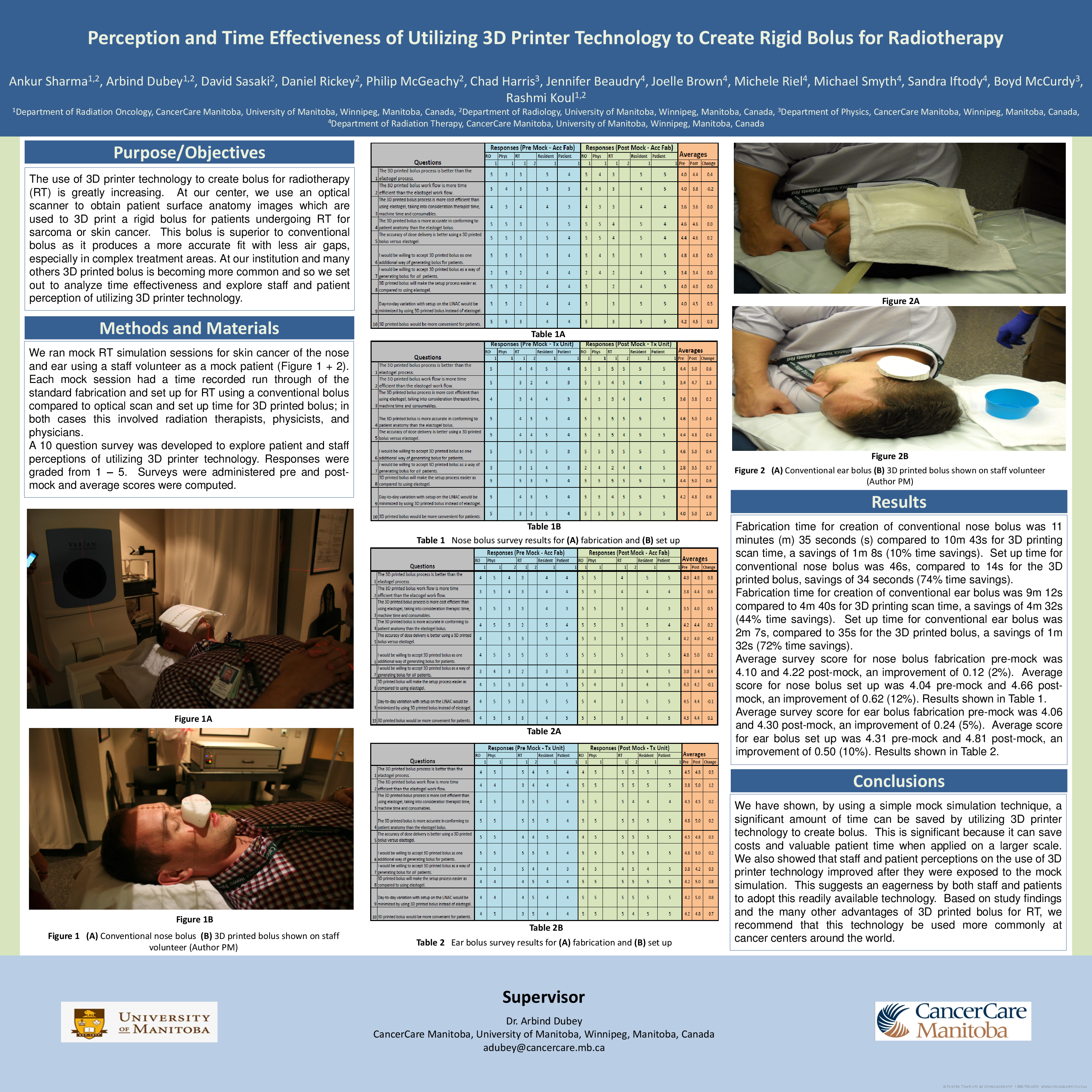
We ran mock RT simulation sessions for skin cancer of the nose and ear using a staff volunteer as a mock patient. Each mock session had a time recorded run through of the standard fabrication and set up for RT using a conventional bolus compared to optical scan and set up time for 3D printed bolus, in both cases involving radiation therapists, physicists, and physicians.
A ten question survey was developed to explore patient and staff perceptions of utilizing 3D printer technology. Responses were graded from 1 – 5. Surveys were administered pre and post-mock and average scores were computed.
Results
Fabrication time for creation of conventional nose bolus was 11 minutes (m) 35 seconds (s) compared to 10m 43s for 3D printing scan time, a savings of 1m 8s (10% time savings). Set up time for conventional nose bolus was 46s, compared to 14s for the 3D printed bolus, savings of 34 seconds (74% time savings).
Fabrication time for creation of conventional ear bolus was 9m 12s compared to 4m 40s for 3D printing scan time, a savings of 4m 32s (44% time savings). Set up time for conventional ear bolus was 2m 7s, compared to 35s for the 3D printed bolus, as savings of 1m 32s (72% time savings).
Average survey score for nose bolus fabrication pre-mock was 4.10 and 4.22 post-mock, an improvement of 0.12 (2%). Average score for nose bolus set up was 4.04 pre-mock and 4.66 post-mock, an improvement of 0.62 (12%).
Average survey score for ear bolus fabrication pre-mock was 4.06 and 4.30 post-mock, an improvement of 0.24 (5%). Average score for ear bolus set up was 4.31 pre-mock and 4.81 post-mock, an improvement of 0.50 (10%).
Conclusion
We have shown, by using a simple mock simulation technique, a significant amount of time can be saved by utilizing 3D printer technology to create bolus. This is significant because it can save costs and valuable patient time when applied on a larger scale. We also showed that staff and patient perceptions in the use of 3D printer technology improved after they were exposed to the mock simulation. This suggests an eagerness by both staff and patients to adopt this readily available technology. Based on study findings and the many other advantages of 3D printed bolus for RT, we recommend that this technology be used more commonly at cancer centers around the world.