Abstract
Purpose
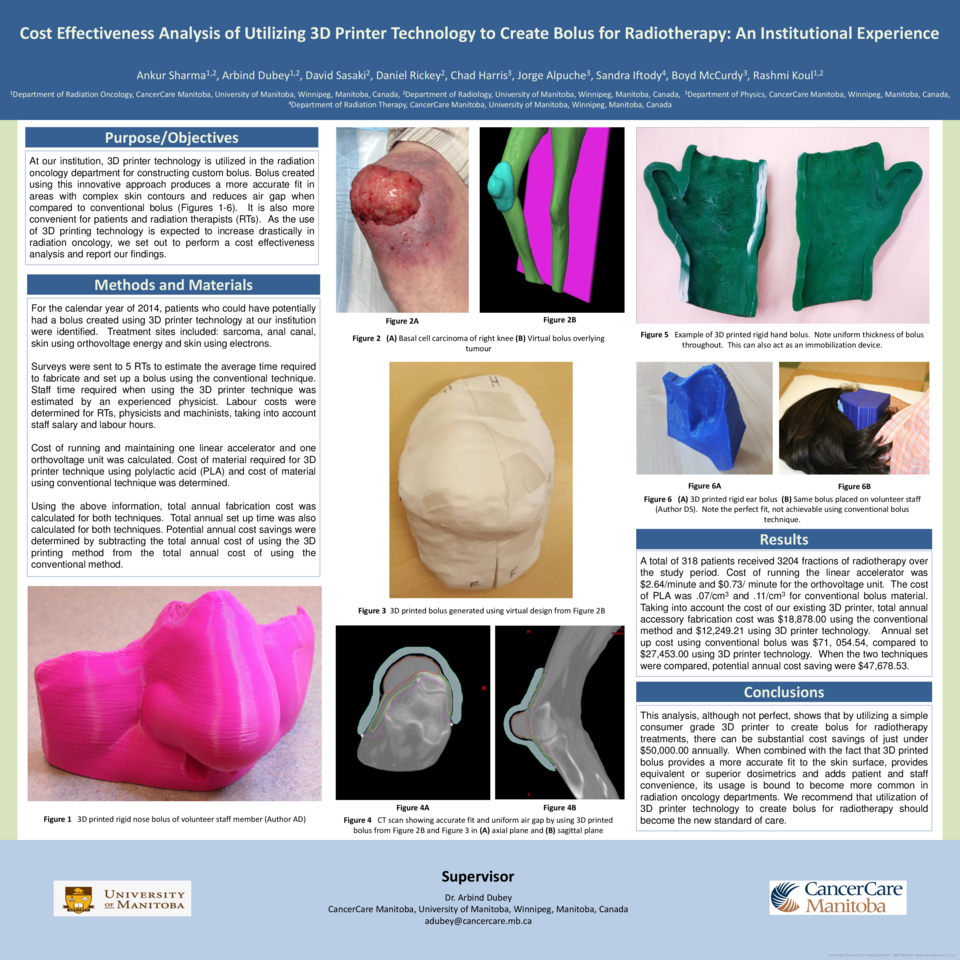
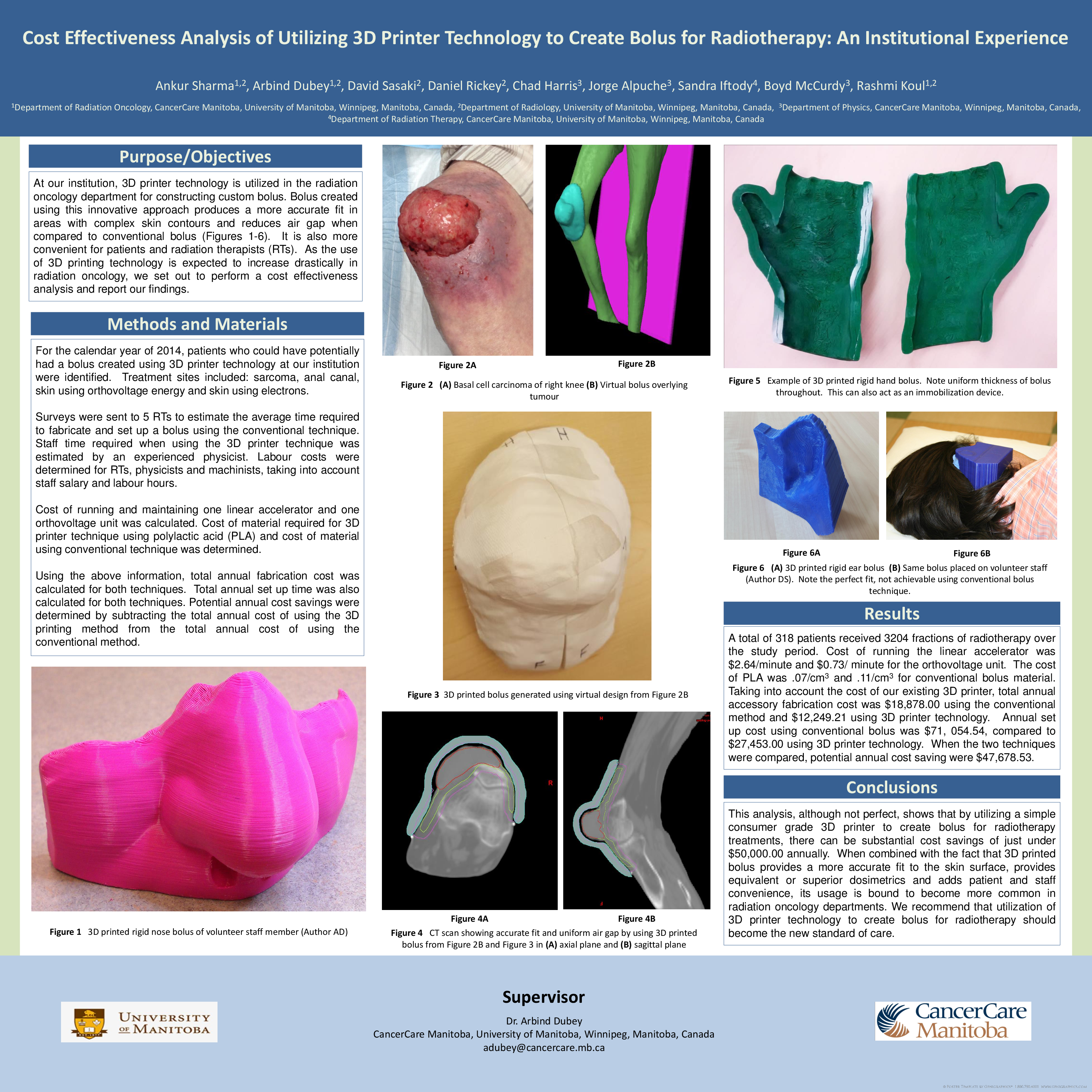
At our institution, 3D printer technology is utilized in the radiation oncology department for constructing custom bolus. Bolus created using this innovative approach produces a more accurate fit in areas with complex skin contours and reduces air gap when compared to conventional bolus. It is also more convenient for patients and radiation therapists (RTs). As the use of 3D printing technology is expected to increase drastically in radiation oncology, we set out to perform a cost effectiveness analysis and report our findings.
Methods
For the calendar year of 2014, patients who could have potentially had a bolus created using 3D printer technology at our institution were identified. Treatment sites included: sarcoma, anal canal, skin using orthovoltage energy and skin using electrons.
Surveys were sent to 5 RTs to estimate the average time required to fabricate and set up a bolus using the conventional technique. Staff time required when using the 3D printer technique was estimated by an experienced physicist. Labour costs were determined for RTs, physicists and machinists, taking into account staff salary and labour hours.
Cost of running and maintaining one linear accelerator and one orthovoltage unit was calculated. Cost of material required for 3D printer technique using polylactic acid (PLA) and cost of material using conventional technique was determined.
Using the above information, total annual fabrication cost was calculated for both techniques. Total annual set up time was also calculated for both techniques. Potential annual cost savings were determined by subtracting the total annual cost of using the 3D printing method from the total annual cost of using the conventional method.
Results
A total of 318 patients received 3204 fractions of radiotherapy. Cost of running the linear accelerator was $2.64/minute and $0.73/ minute for the orthovoltage unit. The cost of PLA was .07/cm3 and .11/cm3 for conventional bolus material. Taking into account the cost of our existing 3D printer, total annual accessory fabrication cost was $18,878.00 using the conventional method and $12,249.21 using 3D printer technology. Annual set up cost using conventional bolus was $71, 054.54, compared to $27,453.00 using 3D printer technology. When the two techniques were compared, potential annual cost saving were $47,678.53.
Conclusions
This analysis, although not perfect, shows that by utilizing a simple consumer grade 3D printer to create bolus for radiotherapy treatments, there can be substantial cost savings of just under $50,000.00 annually. When combined with the fact that 3D printed bolus provides a more accurate fit to the skin surface, provides equivalent or superior dosimetrics and adds patient and staff convenience, its usage is bound to become more common in radiation oncology departments. We recommend that utilization of 3D printer technology to create bolus for radiotherapy should become the new standard of care.