Abstract
Background – Effective basic airway management and mask ventilation are paramount when resuscitating newborn infants1. These skills are usually assessed in protected classroom environments, without the distraction of the clinical setting. There is a paucity of evidence on the effect of distraction on a practitioner’s ability to perform effective mask ventilation during newborn resuscitation2.
Research Question – What is the effect of distraction on mask leak, inspiratory and expiratory time and ventilatory rate when practitioners perform basic mask ventilation on a term and preterm manikin?
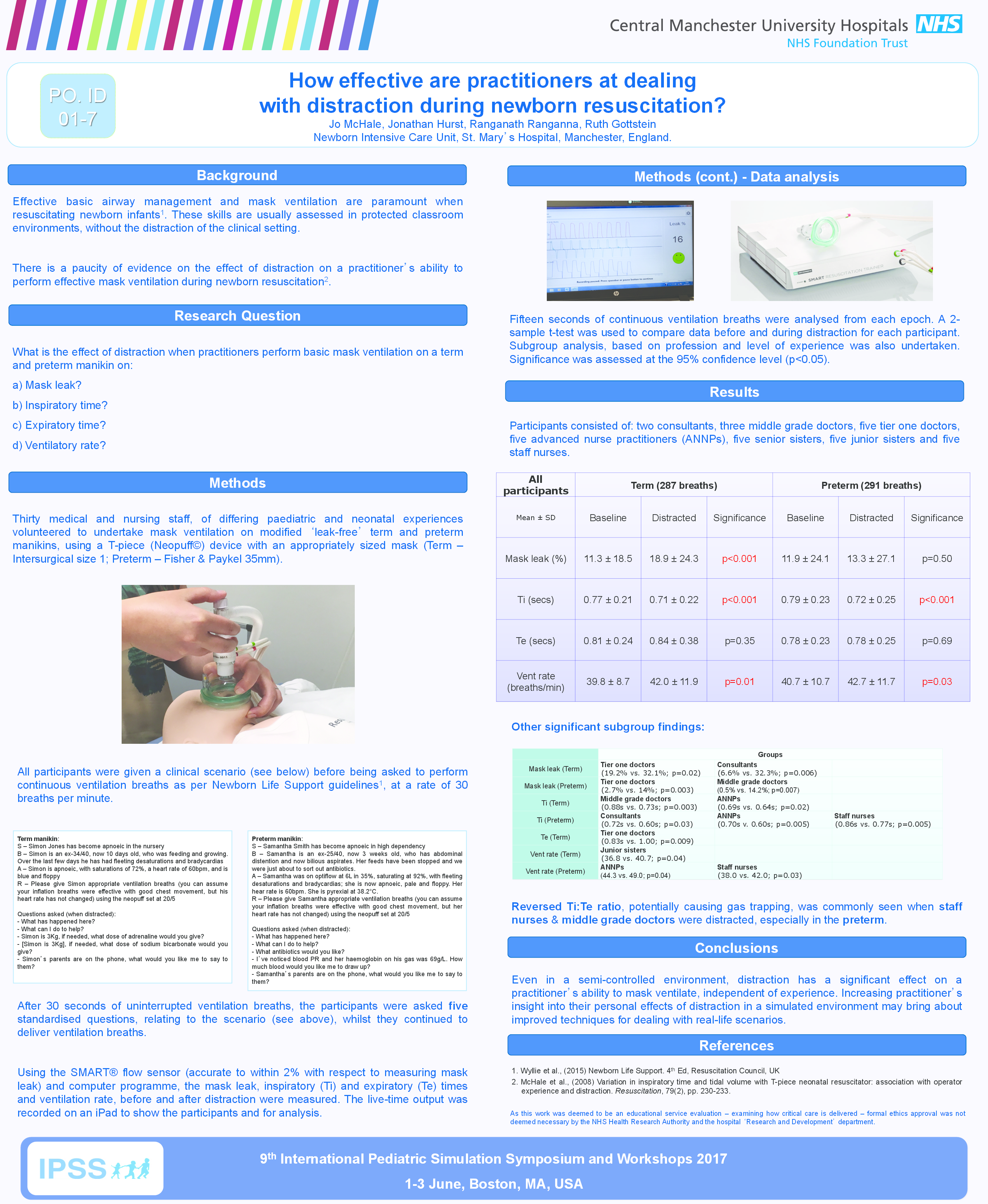
Methodology – Thirty medical and nursing staff, of differing paediatric and neonatal experiences, undertook mask ventilation on modified term and preterm manikins, using a T-piece (Neopuff®) device with an appropriately sized mask. Participants were given a clinical scenario before the test and asked to perform continuous ventilation breaths as per Newborn Life Support guidelines1. After 30 seconds, each participant was asked five standardised questions relating to the scenario, akin to real life questions posed in the clinical setting, whilst they continued to provide ventilation breaths. The mask leak, inspiratory (Ti) and expiratory (Te) time and ventilatory rate, before and during distraction, were calculated using SMART® flow sensor. Fifteen seconds of continuous ventilation breaths were analysed from both epochs. A 2-sample t-test was used to compare data before and during distraction for each participant. A subgroup analysis was performed dependent on the level of experience and participants’ professional backgrounds. Signficance was assessed at the 95% confidence level (p≤0.05).
Results – 2 consultants, 3 middle grade doctors, 5 tier one doctors, 5 advanced nurse practitioners, 5 senior sisters, 5 junior sisters and 5 staff nurses participated. When participants were analysed together, in the term infant (287 breaths analysed), there is a significant difference in mask leak (11.3% versus 18.9%, p<0.001), shortened Ti (0.77s versus 0.71s, p<0.001) and increased in frequency of delivered breaths (39.8 versus 42.0 breaths/min; p=0.01) when distracted. In the preterm infant (291 breaths analysed), Ti is significantly shortened (0.79s versus 0.72s, p<0.001), ventilation rate increased (40.7 versus 42.7 breaths/min, p=0.03) and shortening of the inspiratory:expiratory time ratio, commonly reversed when junior nurses were distracted.
Conclusion – Even in a semi-controlled environment, distraction has a significant effect on a practitioner’s ability to mask ventilate Increasing practitioner’s insight into their personal effects of distraction in a simulated environment may bring about improved techniques for dealing with real-life scenarios.