Abstract
Background: Simulation-based training may improve healthcare value by improving outcomes and minimizing complications. However, there is limited information regarding the cost-effectiveness of simulation curricula. The purpose of this study was to estimate the cost effectiveness of simulation training aimed at reducing cast saw injuries by orthopaedic surgery residents.
Research Question: What is the clinical efficacy and return-on-investment (ROI) of simulation-based training aimed at reducing cast saw injuries by orthopaedic surgery residents?
Methods: Third-year orthopaedic residents rotating at a children’s hospital underwent simulation-based instruction on distal radius fracture (DRF) reduction, casting, and cast removal using an oscillating saw. The incidence of cast saw injuries was analyzed before and after implementation of the simulation curriculum. Actual and potential costs associated with cast saw injuries included wound care, extra clinical visits, and medicolegal expenses (indemnity payments and legal expenses). Medicolegal expenses were provided by the Controlled Risk Insurance Company (CRICO), the medical malpractice insurer for the Harvard medical community. Curriculum costs were calculated using time-derived activity-based accounting methodology. The costs of cast saw injury and the simulation curriculum were compared to determine overall savings and return-on-investment (ROI).
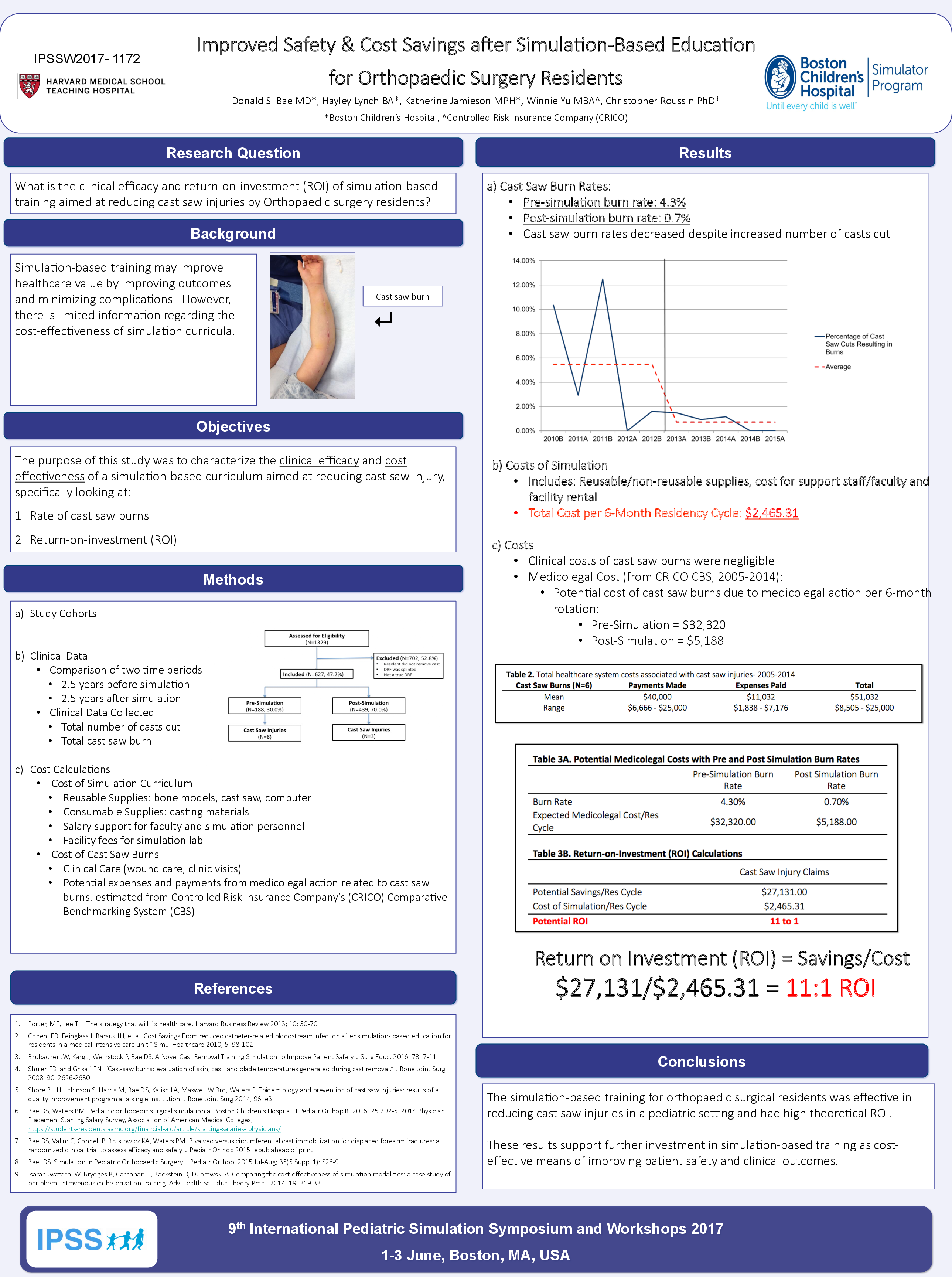
Results: In the 2.5 years prior to simulation, cast saw injuries occurred at a rate of approximately 4.3 per 100 casts cut by orthopaedic residents. For the 2.5-year period post-simulation, the cast saw injury rate decreased to approximately 0.7 per 100 casts cut (p=0.002). The total cost to implement the casting simulation-based workshop was $2,465.31 per 6-month resident rotation. Actual costs attributed to cast saw injuries per resident rotation were $65.83 before simulation, and negligible after simulation. Based on historical data, the potential total payment (claims) related to improper casting technique or cast saw burn that resulted in payment (n=13) ranged from $2,023 and $99,373 per claim. The anticipated savings from averted cast saw injuries and associated medicolegal payments in the 2.5 years post-simulation was $27,131, representing an 11 to 1 ROI. Maximum potential savings were estimated at $104,594 with potential return of 42 to 1.
Conclusions: The simulation-based training for orthopaedic surgical residents was effective in reducing cast saw injuries in a pediatric setting and had high theoretical ROI. These results support further investment in simulation-based training as cost-effective means of improving patient safety and clinical outcomes.
Key Words: Cost-effectiveness, Cast Saw Burns, Orthopaedics.