Abstract
Background:
Extracorporeal cardiopulmonary resuscitation (ECPR) is an essential, lifesaving therapeutic service provided by most modern cardiac intensive care units. Successful outcome after ECPR depends on a coordinated multidisciplinary effort leading to deployment onto extracorporeal life support in the shortest possible duration, with minimal procedural disruptions while maintaining adequate quality of cardiopulmonary resuscitation. ECPR is an extremely stressful clinical intervention. The infrequency of ECPR necessitates continuous education of all involved personnel to attain a level of preparedness that would ensure optimal ECPR when the situation is actually encountered in the unit. We have designed and implemented a novel, structured protocol-based educational tool for patient care providers utilizing simulation-based training sessions to develop and maintain competency in ECPR.
Methods:
The simulation protocol was designed with specific, realistic, and achievable learning objectives. The goal of the simulation was to familiarize bedside staff with the process of initiation of ECPR, the patient and room set up necessary for uneventful cannulation, and the various ancillary paraphernalia required for the procedure. Emphasis was also placed on the importance of role-based communication during ECPR to minimize the chaos that is often seen during a sudden, unanticipated life-threatening patient event. The protocol was finalized after receiving input from the bedside staff, as well as the educators, to maximize the yield from these sessions.
A trial practice session was conducted to assess feasibility and flow. Each session was intended to start with a pre-brief presentation. This was followed by the actual simulation of an ECPR scenario. A formal debrief concluded the training session. All participants were provided with a feedback form to share their opinion on the usefulness of these simulations and to suggest possible improvements.
Results:
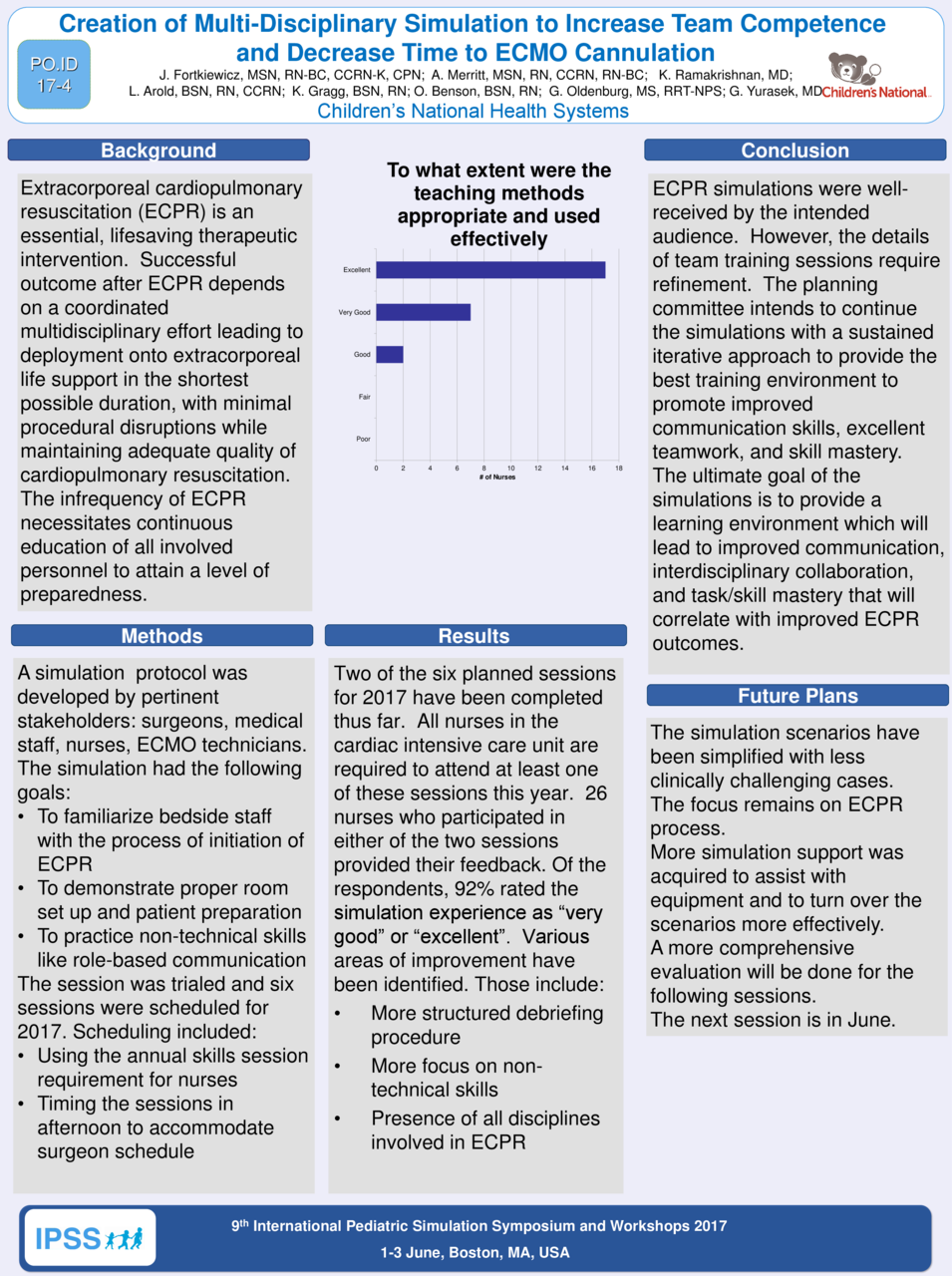
Two of the six planned sessions for 2017 have been completed thus far. All nurses in the cardiac intensive care unit are required to attend at least one of these sessions this year. Twenty-eight nurses who participated in either of the two sessions provided their feedback. Of the respondents, 93% rated the simulation experience as “very good” or “excellent”. Various areas of improvement have been identified, including a more structured debriefing procedure, more focus on non-technical skills, and ensuring inclusive presence of all disciplines involved in ECPR to make the training more team-oriented.
Conclusion:
ECPR simulations were well-received by the intended audience. However, the details of team training sessions require refinement. The planning committee intends to continue the simulations with a sustained iterative approach to provide the best training environment to promote improved communication skills, excellent teamwork, and skill mastery. The ultimate goal of the simulations is to provide a learning environment which will lead to improved communication, interdisciplinary collaboration, and task/skill mastery that will correlate with improved ECPR outcomes.